Journal of caring sciences, 9(3), 162-167; DOI:10.34172/jcs.2020.024
Original Article
Comparison of the Efficacy of Honey Gel and Clotrimazole Cream in the Treatment of Vaginal Candidiasis Signs: A Randomized Clinical Trial
Zahra Seifinadergoli1, Fatemeh Nahidi1,*, Abdolrasoul safaiyan2, Yousef Javadzadeh3, Tahereh Eteraf oskouei4
1
Department of Midwifery & Reproductive Health, School of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2
Department of Biostatistics and Epidemiology, Faculty of Health, Road Traffic Center, Tabriz University of Medical Sciences, Tabriz, Iran
3
Biotechnology Research Center, Faculty of Pharmacy, Tabriz University of Medical Sciences, Tabriz, Iran
4
Department of Pharmacology and Toxicology, Faculty of Pharmacy, Tabriz University of Medical Sciences, Tabriz, Iran
Email: nahidifateme@yahoo.com
© 2020 The Author(s).
Abstract
Introduction: Due to the increasing resistance to synthetic antifungal drugs, the use of drugs with a natural origin, with low side effects and low prices is a priority. This study was performed to evaluate the effect of topical honey gel and clotrimazole cream in treatment of signs of vaginal candidiasis.
Methods: This randomized clinical trial was conducted to evaluate the topical use of honey and clotrimazole in the signs of vulvovaginal candidiasis in clinics and medical centers in Tabriz. The study was performed on 106 non-pregnant women (18 to 45 years old) who had clinical signs of candidiasis. Patients were randomly divided into two groups receiving honey gel and clotrimazole vaginal cream (53 people per group). Each group was treated for 8 days. Before, 4, and 8 days after the intervention, patients recorded the sings of disease and possible side effects of drugs using a researcher-made questionnaire. The results were analyzed using SPSS software ver. 22. Inter-group comparison was carried out using McNemar, Cochran Q and independent t-tests. P-value < 0.05 was considered statistically significant.
Results: In the three evaluation periods, a significant reduction in the sings was observed compared to the before starting of treatment regimes. The results of the cultures were similar and there was no significant difference between the two honey gel and clotrimazole cream groups.
Conclusions: Our results may suggest that honey gel could have promising benefits in the treatment of vulvovaginal candidiasis as the main drug or as an adjunct to other antifungal drugs.
Keywords: Honey, Clotrimazole, Vulvovaginal Candidiasis, Signs
Introduction
Candida albicans is responsible for 85% to 95% of vaginal yeast infections.1 Factors that cause an increased susceptibility to vulvovaginitis candidiasis (VVC) include: antibiotic therapy, pregnancy, uncontrolled diabetes mellitus, using oral contraceptives (especially high-dose formulations), immune suppressants, and synthetic clothing.1-4 The most common signs of vaginal candidiasis are discharge, may be aqueous to thick and homogenous. There are vaginal burning, burning and sensitivity of the vulva.1,4,5 Treatment agents include butoconazole, clotrimazole, miconazole and terconazole. The side effects of these treatments are headache, gastrointestinal disorders.6-8,
The incidence of Candida infections is escalating worldwide. The serious nature of these infections is compounded by increasing levels of drug resistance.4 The increase in the resistance of antifungal has attracted the attention of the scientific community.8
Honey as a medicine is being used thousands of years. If it is used alone or in combination with other substances in vagina to inhibit the growth of Candida laboratory and clinical results of honey in inhibiting the growth of various fungi such as Candida has been promising.9-14 In Islam, honey strongly recommended for healing purposes. However, honey has a low use in modern medicine result of lack of scientific support, it has been observed that honey can be used to treatment liver, cardiovascular and gastrointestinal problems. Ancient Egyptians, Assyrians, Chinese, Greeks and Romans used honey for wounds and diseases of the intestine. Natural honey has bactericidal activity against many organisms including Salmonella, Shigella, Escherichia coli, Helicobacter pylori , etc.15,16
Different types of honey were able to inhibit bacterial growth.17 Honey is very effective in clearing infection in wounds and protecting them from becoming infected.9 In a study conducted on 129 women with VVC, honey combined with yoghurt was more effective in treatment of clinical signs compared to azoles compositions.18 Honey also has showed a positive healing effect in combination with other substances such as starch.9,19 Considering that the effect of pure honey on candida albicans has only been studied in-vitro, and not in clinical settings, and given side-effects of chemical drugs, and resistance against antifungal drugs in many patients.20-23 This study was conducted to examine the effects of vaginal honey gel and clotrimazole cream in treatment of vaginal candidiasis sign. The result of this study can helpful to find an effective medicine with fewer side-effects.
Materials and Methods
The research hypothesis was that vaginal honey gel is as effective as vaginal clotrimazole cream in the treatment of candidiasis signs. The target population consisted of women with vaginal discharge, and burning and sensitivity of the vulva, and vaginal burning, who were referred to the selected health centers in Tabriz (5/55/6629, date:11, 2014). A total of 300 potential patients were recruited in the study, out of which 190 patients were eliminated. Finally, 110 patients with positive culture and clinical signs were randomly divided into honey and clotrimazole groups. During the study, four participants (2 from the intervention group and 2 from the control group) were excluded due to lack of follow-up. The sample size was calculated to be 106, by assuming a power of 95% and confidence level of 95% by using program available at http://www.openEpi.com18 considering the test power, 0.95, and P represents the probability of the main outcome (P1= 0.68 , P2= 0.94).24 Consequently, the study was performed on a total of 106 patients (53 per group).
The inclusion criteria were as follows: 1) age range, 18-45 years; 2) signs of vaginal candidiasis, based on interviews, observation, and laboratory studies; 3) no pregnant women who had not used any immune suppressors or broad-spectrum antibiotics in the past month; and 4) no history of epilepsy, diabetes, cardiac diseases, hypertension, thyroid diseases, or advanced arthritis. On the other hand, the exclusion criteria were: 1) pregnancy during the study; 2) unwillingness to continue participation in the study; 3) necessity to use antibiotics during the study; 4) allergy to medicines; and 5) failure to follow the instructions (negligent use of drugs for more than one night).
In this study, the honey was provided from Sabalan mountains around Ardebil city, whose purity and microbial tests had been determined by experts from Tabriz Agricultural Jihad. All formulation stages of honey gel were performed in the laboratory by a Professor of Pharmaceutics of Tabriz School of Pharmacy. The honey used contained 0.83% of saccharose, which complied with the international standards (maximum 5%), with fructose to glucose ratio of 1.78, which was normal compared to standard value (minimum 0.9). This honey also had an acceptable level of microbes. To prepare vaginal honey gel 50%, first, preserved water was prepared using methyl paraben 2% and propyl paraben 0.02%, and 1% of carbomer 934 was added to some of this water, and gently stirred until fully dissolved. Next, right amounts of honey were gently added, and after full dispersion, the remaining water was added and stirred. The final gel was produced by addition of tri-ethanol-amine in drops. The prepared honey gel was poured into unlabeled sterile tubes using a filling device. Clotrimazole 1% cream also poured into similar sterile tubes. These tubes were coded A (honey gel) and B (clotrimazole cream) by the pharmaceutics professor. Demographic information, including information related to age, family size, socioeconomic status, education, and occupation, was collected through a questionnaire. The researcher was taught how to perform culture and interpret results by a laboratory technician over two months. Concentration of honey was determined 30% based on stability of the gel. To observe ethical considerations, and because honey gel was being used for the first time on human mucosa, it was initially tested on 30 samples with positive candidiasis in a pilot study. Patients recovered from clinical symptoms after 8 days; yet, the majority still showed positive cultures. Hence, study was performed with increased concentration of honey to 50%. Patients were provided with explanations about study. Then, they were examined, and samples were taken from them. Those with signs of vaginitis that met inclusion criteria completed a preliminary questionnaire. A disposable speculum was used without lubricant to take samples, and signs of disease were recorded in observation checklist. Samples of vaginal discharge were taken using two sterile cotton swabs. The first swab was smeared over two slides; 1-2 drops of normal saline were poured on the first, and KOH 10% solution was poured on the second. The first slide was examined under a microscope at 10X magnification. Observation of key cells or flagellate parasites and amine odor in Whiff test meant diagnosis of Gardenella or Trichomonas , and exclusion from study. The second slide was also examined under the same microscope, and observation of mycelium and blastospores meant positive smear test for candida. Next, vaginal discharge was assessed using pH paper, and pH less than 4-4.5, which confirmed candida infection was recorded in observation checklist. Kappa coefficient of agreement was calculated for all cases (minimum agreement coefficient was 0.8). Otherwise, the sample was excluded from study with mixed infection diagnosis. The second swab showing positive smear for candida was sent to the laboratory in a tube containing normal saline to be transferred to fungi culture medium of Dextrose Agar for final diagnosis of candida species. Culture medium was prepared by the researcher according to manufacturer’s instructions, and in sterile conditions, 20 mL was poured onto each 8-mm sterile plate. Afterward, the researcher prepared streak culture of the samples on culture medium. Samples cultured on Dextrose Agar were incubated at 30-37°C for 48 to 72 hours, and colonies were examined under microscope after 72 hours by the researcher, supervised by a laboratory technician. Next, positive cultures for fungi were removed and poured into tubes containing human serum using a loop; in case of growth, presence of candida albicans was confirmed. All species of candida were included in the study. Samples were then randomly coded, using randomization software. Participants were divided into honey gel (A) and clotrimazole cream (B) groups. Patients received 5 g of 50% honey gel and 5 g of 1% clotrimazole cream using an applicator every night for 8 nights. Subjects, were unaware of the content of packages. All patients were provided with instructions of use and hygiene recommendations. They were also advised not to have sex without condoms, and avoid vaginal showers, use of other vaginal medications and antibiotics. Patients with confirmed test results showing fungal growth on culture medium and confirmed candida were contacted and asked to visit the clinic four days after commencement of use of medication. Patients’ compliance with hygiene instructions and any serious complication were assessed.
In the follow-up stage after completion of treatment, patients were examined in terms of microscopic and other symptoms and results were recorded in the observation checklist. Then, a second culture was prepared to ensure patients’ recovery or otherwise, and results were recorded in the observation checklist. Data were analyzed by using Cochran Q and independent t tests using SPSS 22 statistical software and P < 0.05 considered as significant level. If treatment in the honey gel group failed, patients were requested to attend the clinic the following day to receive routine treatment with clotrimazole cream for 8 days.
Single-blinded method was used for blinding and 106 subjects with positive culture was divided to two groups (n=53) with using NCSS PASS V11 software.
The results obtained were analyzed and compared in Independent t tests at the beginning of the study and After collecting data and entering in SPSS software 22 (IBM© Corp., Armonk, NY, USA), at 3-time intervals (baseline, 4 days after the intervention and 8 days after the intervention). Outlier data were recognized by Box plot test and normality was checked by Kolmogorov–Smirnov test. For comparing two groups the data were analyzed by using McNamara test, Cochran Q-test. P value less than 0.05 was considered statistically significant.
All 300 patients participating in this study signed the informed consents.
Results
A total of 300 potential patients were recruited in the study, out of which 190 patients were eliminated. Finally, 110 patients with positive culture and clinical signs were randomly divided into honey and clotrimazole groups. During the study, four participants (2 from the intervention group and 2 from the control group) were excluded due to lack of follow-up (Figure 1).
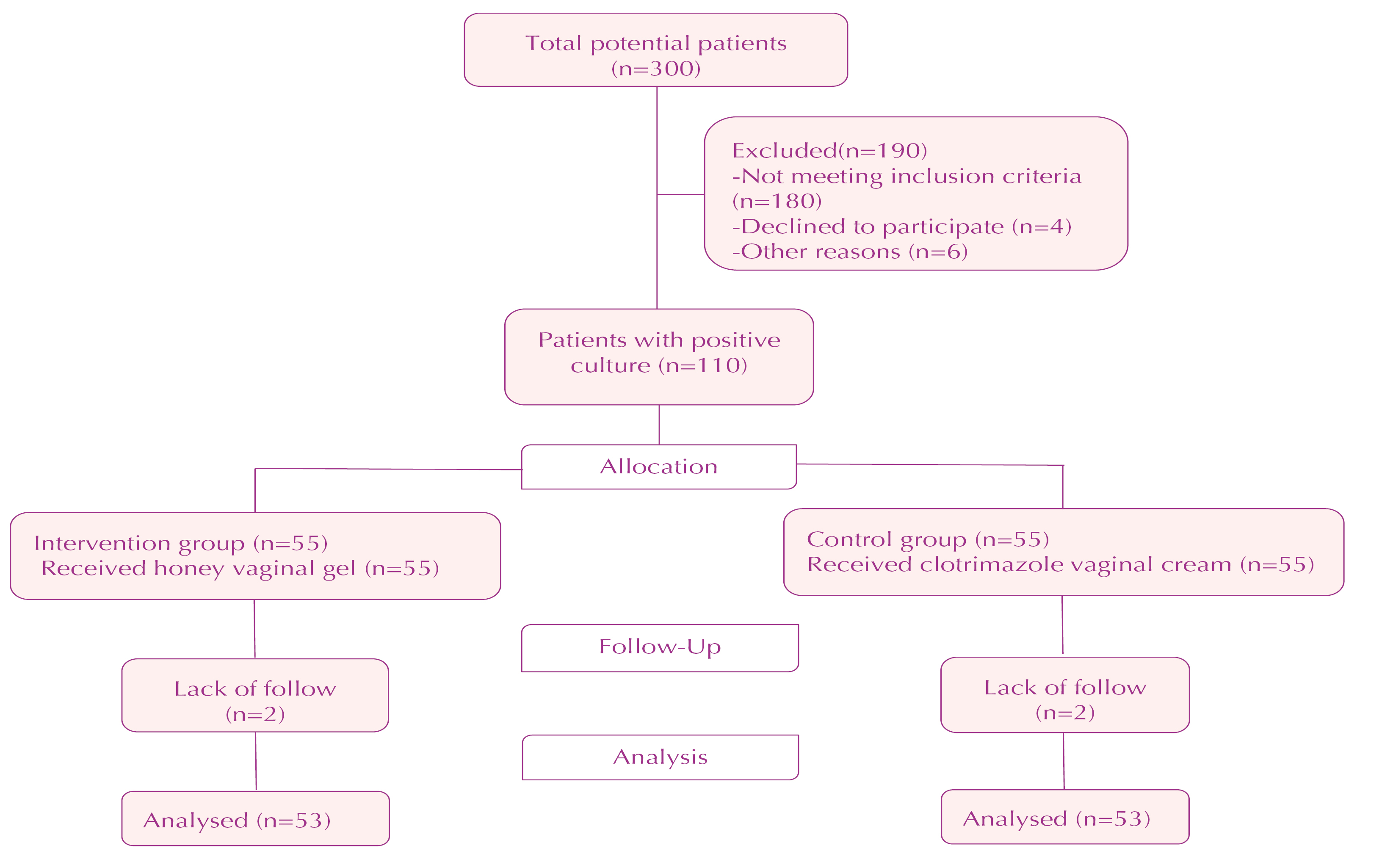
Figure 1. Flow chart of the study.
No significant difference was found between honey and clotrimazole groups in terms of quantitative demographic parameters such as age, spouse’s age, household size, gravida, parity, live births, frequency of sex per week, weight, body mass index, and qualitative demographic parameters such as mother’s education, father’s education, house ownership, alcohol and cigarette use, cesarean section or miscarriage, menstruation, and previous history of infection (P > 0.05). IUD was used as a contraceptive in 60% of patients in honey group and 74% in clotrimazole group. According to chi-square test, two groups were not significantly different in terms of type of contraception method (P < 0.001) (Table 1).
|
Table 1. Characteristics of women in terms of honey and clotrimazole groups’ variables
|
|
Groups
|
Honey
|
Clotrimazole
|
P
value
|
|
Variables
|
Mean (SE)
|
Mean (SE)
|
| Age |
30.72 (0.82) |
29.74 (1) |
0.44 |
| Age of husband |
34.23 (0.86) |
33.17 (0.91) |
0.40 |
| Number of family |
4.51 (0.26) |
4.02 (0.16) |
0.11 |
| Number of pregnancies |
2.21 (0.17) |
2.06 (0.15) |
0.50 |
| Number of deliveries |
2.08 (0.16) |
2 (0.15) |
0.72 |
| Number of alive child’s |
2.09 (0.16) |
2 (0.15) |
0.66 |
| Sexing week |
2.32 (0.11) |
2.13 (0.12) |
0.23 |
| Weight (g) |
66.77 (1.44) |
63.49 (0.98) |
0.06 |
| Height (cm) |
158.94 (0.74) |
157.85 (0.53) |
0.23 |
| BMI |
26.45 (0.56) |
25.51 (0.41) |
0.17 |
| Surface home |
2.45 (0.07) |
2.45 (0.07) |
1.00 |
|
BMI, body mass index; SE, standard error.
|
Table 2 shows the effects of honey gel and clotrimazole cream on signs of vaginal candidiasis on the three occasions. Comparing differences in signs before treatment and after completion of treatment McNemar test showed a reduction in candidial vaginal discharge in honey group (P =0.00), but had not changed in clotrimazole group and no difference was observed between the two groups in sensitivity and burning vulva (P > 0.05). So sensitivity and burning volva in two groups has reducted. McNemar test showed no difference in burning vaginal in honey group but showed a reduction in clotrimazole group.
|
Table 2. Differences between honey gel and clotrimazole cream in their effects on signs
|
|
Signs of vaginal candidiasis
|
Groups
|
Before treatment
No. (%)
|
Forth days after treatment
No. (%)
|
Eighth days after treatment
No. (%)
|
P
value
a
|
P
value
b
|
|
Groups
|
Time
|
Vaginal candida
discharge |
Honey |
53 (100) |
53 (100) |
25 (47) |
0.001 |
0.01 |
0.000* |
|
Clotrimazole |
53 (100) |
53 (100) |
13 (25) |
0.000 |
|
|
| Burning and sensitivity of the vulva |
Honey |
11 (21) |
0 (0) |
0 (0) |
0.000 |
0.18 |
0.000* |
|
Clotrimazole |
6 (11) |
0 (0) |
0 (0) |
0.002 |
|
|
| Vaginal burning |
Honey |
1 (2) |
1 (2) |
0 (0) |
0.607 |
0.07 |
0.000* |
|
Clotrimazole |
7 (13) |
0 (0) |
0 (0) |
0.001 |
|
|
| Culture results |
Honey |
53 (100) |
- |
27 (50) |
0.001 |
0.22 |
0<001* |
|
Clotrimazole |
53 (100) |
- |
10 (20) |
0.001 |
|
|
|
aMcNemar-test, bCochran Q- test, *Statically significant.
|
Cochran Q test showed a reduction in discharge, burning in both groups.
Cochran Q test showed a significant reduction in frequency of culture medium (Sabouraud dextrose agar) due to application of honey and clotrimazole after treatment (Table 2).
Discussion
Results of the current study indicated the antifungal effect of honey, like clotrimazole, on vaginitis signs. Similar results were also observed in a study by Darvishi et al., that they compared the antifungal effect of honey plus yogurt with clotrimazole on vaginitis.25 Abdelmonem et al., also reported similar results regarding the antifungal effect of honey plus yogurt compared with that of tioconazole.18
The obtained results indicate that sign of burning and sensitivity of the vulva after taking 8 day a vaginal gel honey and clotrimazole is reduced significantly. In this regard, results of the study Darvishi et al., showed that recovery in term of vaginal candida discharge in 7 days after treating with honey and yogurt mixture happened in more than ¾ samples and in clotrimazole group occurred in almost two-thirds of the cases.25 That was not similar with current study. In addition to study results of Abdelmonem et al., 129 pregnant women with vulvovaginitis candidiasis suggests that the use of yogurt and honey mixture in comparison with itraconazole group improves signs of VVC. So that secretions, and redness of the vulva and vagina, has significantly decreased in consumer group of vaginal cream yogurt and honey compared to itraconazole group.18 That it was the same with current study.
It is assumed that antifungal and anti-inflammatory effect of honey is that make vaginal environment unsuitable for the growth of candidiasis. The honey through producing the prostaglandins reduces the edema and pain in the inflammatory tissues. In the current study honey cause inhabitation of colonization of Candida species which is consistent with the findings of the study of others.26-32, This effect is likely related to the antimicrobial effect of honey is due to its osmolality. The present findings demonstrate the effectiveness of honey on negative cultures of samples within 8 days after the intervention, while no effect was observed in the study of Shalev et al.27 It is assumed that difference is due to antimicrobial effect of honey. The culture results of the two groups were similar after treatment that it was the same with Rasooli et al.33 The limitations of this study can be mentioned relatively short follow-up period. Subject loss during the investigation, lack of return of some subjects for culture after treatment were other. The strengths point of present study is assessment of signs and comparison of two treatment methods and having a control group, designing the study in single-blind and randomized into two groups of samples.
Conclusion
In the current study administration of honey and clotrimazole had equal effects in turning positive culture into a negative one and honey has desired effect in the treatment of burning and sensitivity of the vulva. It is more economical in terms of costs, and do not have the synthetic drugs side effects. Therefore its use in combination with topical formulations for the treatment of vaginal candidiasis signs would be useful.
The current study provided a novel drug which was natural, available, cheap, easy to be prepared, easy to be used. The gel produced a high clinical cure rate in patient with VVC.
The honey gel is a complementary or an alternative therapy to antifungal agents if they are ineffective. The authors hope that this gel may add more to the field of complementary medicine. Future studies should be conducted with the intent to investigate the effects of honey on other vaginal infections and in various age groups.
Acknowledgements
This paper is a part of MS thesis, which has been supported by International branch of Shahid Beheshti and Tabriz University of Medical Sciences. These organization and study participant.
Ethical Issues
The ethical regulations dictated in the act provided by Shahid Beheshti University of Medical Sciences and Tabriz University of Medical Sciences (ref. no. of the ethics approval from Shahid- Beheshti University of Medical Sciences: 1000/2577, date: January 05, 2015) were strictly observed. This study was registered in the Iranian Registry of Clinical Trials (http://www.irct.ir ) with the registration code IRCT201604144317N9.
Conflict of Interest
The authors declare no conflict of interest in this study.
Author’s Contributions
Study conception and design, data collection: ZS. Critical revision of the article and drafted the manuscript: FN and ZS; Data analysis and interpretation: AS; Honey gel formulation: YJ; Treatment protocols design and Scientific advisor: TEO.
Research Highlights
|
|
What is the current knowledge?
The effect of pure honey on candida albicans has only been studied in-vitro, and not in clinical settings.
What is new here?
The current study provided a novel drug which was natural, available, cheap, easy to be prepared, easy to be used. Honey gel produced a formulation for the treatment of vaginal candidiasis signs would be useful with VVC.
|
References
- Berek JS. Berek and Novak’s gynecology. 15th ed. Philadelphia: Wolters Kluwer; 2012.
- Kačániová M, Melich M, Kňazovická V, Felšöciová S, Sudzinová J. The antimicrobial activity of honey and propolis against yeasts Candida species. Scientific Papers Animal Science and Biotechnologies 2009; 42(2): 167-73.
- Weitzner JS. Danforth’s obstetrics and gynecology. N Engl J Med 1990; 323(7): 493-4. doi: 10.1056/nejm199008163230723. [Crossref]
- Banaeian-Borujeni S, Mobini GR, Pourgheysari B, Validi M. Comparison of the effect of honey and miconazole against Candida albicans in vitro. Adv Biomed Res 2013; 2: 57. doi: 10.4103/2277-9175.115800. [Crossref]
- Borisov I, Kolarov G, Bobcheva S, Ivanova A. Treatment of chronic recurrent vulvovaginal candidiasis with fluconazole (fungolon--Actavis). Akush Ginekol (Sofiia) 2005; 44 Suppl 2: 17-20. [Bulgarian].
- Jurmain R, Kilgore L, Trevathan W, Bartelink E. Essentials of physical anthropology. 10th ed. United States, Wadsworth: Cengage Learning; 2016.
- Cathleen E, Morrow MD. Gynecology for the primary care physician. JAMA 2008; 300(19): 2312-3. doi:10.1001/jama.2008.634. [Crossref]
- Moussa A, Noureddine D, Saad A, Abdelmelek M, Abdelkader B. Antifungal activity of four honeys of different types from Algeria against pathogenic yeast: Candida albicans and Rhodotorula sp. Asian Pac J Trop Biomed 2012; 2(7): 554-7. doi: 10.1016/s2221-1691(12)60096-3. [Crossref]
- Muli EM, Maingi JM, Macharia J. Antimicrobial properties of propolis and honey from the Kenyan stingless bee, dactylurina schimidti. Apiacta 2008; 43: 49-61.
- Boukraâ L, Bouchegrane S. Additive action of honey and starch against Candida albicans and Aspergillus niger. Rev Iberoam Micol 2007; 24(4): 309-11. doi: 10.1016/s1130-1406(07)70062-1. [Crossref]
- Shehu A, Ismail S, Rohin MAK, Harun A, Aziz AA, Haque M. Antifungal properties of Malaysian tualang honey and stingless bee propolis against Candida albicans and Cryptococcus neoformans. J Appl Pharm Sci 2016; 6(2): 44-50. doi: 10.7324/japs.2016.60206. [Crossref]
- Gavanji S, Larki B. Comparative effect of propolis of honey bee and some herbal extracts on Candida albicans. Chin J Integr Med 2017; 23(3): 201-7. doi: 10.1007/s11655-015-2074-9. [Crossref]
- Ansari MJ, Al-Ghamdi A, Usmani S, Al-Waili NS, Sharma D, Nuru A, et al. Effect of jujube honey on Candida albicans growth and biofilm formation. Arch Med Res 2013; 44(5): 352-60. doi: 10.1016/j.arcmed.2013.06.003. [Crossref]
- Al-Waili N, Al-Ghamdi A, Ansari MJ, Al-Attal Y, Salom K. Synergistic effects of honey and propolis toward drug multi-resistant Staphylococcus aureus, Escherichia coli and Candida albicans isolates in single and polymicrobial cultures. Int J Med Sci 2012; 9(9): 793-800. doi: 10.7150/ijms.4722. [Crossref]
- Eteraf-Oskouei T, Najafi M. Traditional and modern uses of natural honey in human diseases: a review. Iran J Basic Med Sci 2013; 16(6): 731-42.
- Ediriweera ER, Premarathna NY. Medicinal and cosmetic uses of Bee’s Honey - a review. Ayu 2012; 33(2): 178-82. doi: 10.4103/0974-8520.105233. [Crossref]
- Mercan N, Guvensen A, Celik A, Katircioglu H. Antimicrobial activity and pollen composition of honey samples collected from different provinces in Turkey. Nat Prod Res 2007; 21(3): 187-95. doi: 10.1080/14786410600906277. [Crossref]
- Abdelmonem AM, Rasheed SM, Mohamed A. Bee-honey and yogurt: a novel mixture for treating patients with vulvovaginal candidiasis during pregnancy. Arch Gynecol Obstet 2012; 286(1): 109-14. doi: 10.1007/s00404-012-2242-5. [Crossref]
- Boukraa L, Benbarek H, Moussa A. Synergistic action of starch and honey against Candida albicans in correlation with diastase number. Braz J Microbiol 2008; 39(1): 40-3. doi: 10.1590/s1517-838220080001000010. [Crossref]
- Al-Waili NS, Akmal M, Al-Waili FS, Saloom KY, Ali A. The antimicrobial potential of honey from United Arab Emirates on some microbial isolates. Med Sci Monit 2005; 11(12): BR433-8.
- Groll AH, Piscitelli SC, Walsh TJ. Clinical pharmacology of systemic antifungal agents: a comprehensive review of agents in clinical use, current investigational compounds, and putative targets for antifungal drug development. Adv Pharmacol 1998; 44: 343-500. doi: 10.1016/s1054-3589(08)60129-5. [Crossref]
- Khosravi AR, Shokri H, Katiraee F, Ziglari T, Forsi M. Fungicidal potential of different Iranian honeys against some pathogenic Candida species. J Apic Res 2008; 47(4): 256-60. doi: 10.1080/00218839.2008.11101471. [Crossref]
- Basualdo C, Sgroy V, Finola MS, Marioli JM. Comparison of the antibacterial activity of honey from different provenance against bacteria usually isolated from skin wounds. Vet Microbiol 2007; 124(3-4): 375-81. doi: 10.1016/j.vetmic.2007.04.039. [Crossref]
- Ebrahimy F, Dolatian M, Moatar F, Majd HA. Comparison of the therapeutic effects of Garcin(®) and fluconazole on Candida vaginitis. Singapore Med J 2015; 56(10): 567-72. doi: 10.11622/smedj.2015153. [Crossref]
- Darvishi M, Jahdi F, Hamzegardeshi Z, Goodarzi S, Vahedi M. The comparison of vaginal cream of mixing yogurt, honey and clotrimazole on symptoms of vaginal candidiasis. Glob J Health Sci 2015; 7(6): 108-16. doi: 10.5539/gjhs.v7n6p108. [Crossref]
- Bluestein D, Rutledge C, Lumsden L. Predicting the occurrence of antibiotic-induced candidal vaginitis (AICV). Fam Pract Res J 1991; 11(3): 319-26.
- Shalev E, Battino S, Weiner E, Colodner R, Keness Y. Ingestion of yogurt containing Lactobacillus acidophilus compared with pasteurized yogurt as prophylaxis for recurrent candidal vaginitis and bacterial vaginosis. Arch Fam Med 1996; 5(10): 593-6. doi: 10.1001/archfami.5.10.593. [Crossref]
- Al-Waili NS, Saloom KY. Effects of topical honey on post-operative wound infections due to gram positive and gram negative bacteria following caesarean sections and hysterectomies. Eur J Med Res 1999; 4(3): 126-30.
- Subrahmanyam M. Topical application of honey for burn wound treatment - an overview. Ann Burns Fire Disasters 2007; 20(3): 137-9.
- Biswal BM, Zakaria A, Ahmad NM. Topical application of honey in the management of radiation mucositis: a preliminary study. Support Care Cancer 2003; 11(4): 242-8. doi: 10.1007/s00520-003-0443-y. [Crossref]
- Al-Waili NS. Clinical and mycological benefits of topical application of honey, olive oil and beeswax in diaper dermatitis. Clin Microbiol Infect 2005; 11(2): 160-3. doi: 10.1111/j.1469-0691.2004.01013.x. [Crossref]
- Karimi FZ, Maleki-Saghooni, Heidarian Miri H, Moeindarbari S, Yazdi Moghaddam H. Effect of honey and yogurt on vaginitis candidiasis: a systematic review and meta-analysis of clinical trials. Scientific Journal of Kurdistan University of Medical Sciences 2019; 102: 105-19. [Persian].
- Rasooli T, Nahidi F, Mojab F, Nasiri M, Parsapour H. Effect of honey cinnamon vaginal cream and clotrimazole vaginal cream on improvement of candida vaginitis symptoms in women: randomized clinical trial. Iran J Obstet Gynecol Infertil 2019; 22(3): 59-67. doi: 10.22038/ijogi.2019.13394. [Persian]. [Crossref]