Journal of caring sciences. 12(4):235-240.
doi: 10.34172/jcs.2023.30700
Original Article
Comparison of Vascular Complications after Arterial Sheath Removal using Manual Compression Method and ClampEase Method in Patients Undergoing Coronary Angiography
Javad Kazemi Darafshani Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Seyyed Abbas Hosseini Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 2, * 
Sima Babaei Conceptualization, Formal analysis, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 3 
Alireza Khosravi Farsani Conceptualization, Funding acquisition, Methodology, 4 
Author information:
1Student Research Committee, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran
2Department of Adult Health Nursing, Isfahan University of Medical Sciences, Isfahan University of Medical Sciences, Isfahan, Iran
3Department of Adult Health Nursing, Isfahan University of Medical Sciences, Isfahan, Iran
4Department of Cardiology, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
Abstract
Introduction:
Angiography stands as the paramount and definitive diagnostic method for coronary artery disease. However, akin to various other invasive procedures, it may carry a multitude of complications. This study sought to assess the incidence of vascular complications post-arterial sheath removal, comparing the use of a ClampEase device against manual compression.
Methods:
This quasi-experimental clinical trial involved patients undergoing angiography at the post-angiography ward in Isfahan, Iran. A total of 91 patients were selected through convenience sampling and randomly assigned to either the manual compression or ClampEase device groups. Monitoring common vascular complications like hemorrhage, hematomas, and ecchymosis occurred up to 24 hours post-arterial sheath removal. Data were collected using a digital scale model DM3, a transparent flexible ruler, and a questionnaire named ‘vascular complications after angiography.’ Analysis was performed using SPSS software version 13.
Results:
Statistical analysis revealed that, when compared to the manual method, compression with the ClampEase device led to fewer vascular complications in patients and a quicker return to homeostasis.
Conclusion:
The findings underscore that the ClampEase method is a safer alternative with fewer vascular complications than the manual compression method. This discovery has implications for reducing hospital costs and length of stay. The ClampEase device is associated with a swifter time to hemostasis, contributing to enhanced patient comfort and acceptance.
Keywords: Coronary angiography, Vascular complications, Manual compression, ClampEase C750
Copyright and License Information
© 2023 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
This study was funded by, Isfahan University of Medical Sciences, Isfahan, Iran
Introduction
Over 15 million cardiac catheterizations and angiographies are annually performed worldwide for diagnostic and therapeutic purposes. Angiography, the most accurate way to show the severity of coronary artery disease, provides specialists with vital information about coronary artery disease and other heart disorders. Similar to other invasive methods, this method might be associated with various complications, including myocardial infarction, stroke, arrhythmia, vascular complications, adverse reaction to contrast media, and death.1 Vascular complications including hemorrhage, hematoma, and ecchymosis are the most common complications of catheterization.2 In numerous studies, the average incidence of these complications has been estimated between 16 and 28%.3 The incidence of the mentioned complications is crucial since they can be associated with fever, pain, immobility, coldness and numbness in the limb, significantly reduced hemoglobin, increased hospital stay length, and even a threat to the patient’s life.2 In addition, complications of coronary angiography can lead to increased hospital costs.4 Nursing care for identifying and preventing such complications is essential due to the prevalence and consequences of vascular complications after angiography.2
Manual compression is the most widely used method of inducing homeostasis.1 However, this method requires discontinuation of anticoagulants and prolonged bed rest. It is also accompanied by patient discomfort and the nurse’s hand fatigue. On the other hand, vascular closure devices provide the patient’s comfort, require less time spent by the nurse, and reduce the time required for homeostasis. However, the safety of these devices is still under investigation.5
The ClampEase C750 device model California is a vascular closure device consisting of a flat metal base with a C-shaped arm clamp attached to a transparent pressure plate.6 When the arterial sheath is removed, the C-shaped arm clamp is lowered so that the transparent base compresses the catheter insertion site. Compression devices are technically efficacious.7
A meta-analysis was conducted by Biancari et al in 2010 on 7528 patients after angiography to evaluate the safety and efficacy of vascular closure devices. The results show that using these devices shortens the achievement of homeostasis; consequently, less recovery time is required, and the patient spends a shorter period in bed. Nevertheless, further studies are needed to obtain more definitive results.8
In this regard, Cox et al carried out another review on 34 randomized controlled trials (RCTs) published up to 2015 that compared vascular closure devices with manual compression. The results showed that patients for whom a vascular closure device was used needed a shorter time for achieving homeostasis, getting out of bed and being discharged compared to those for whom the manual method was used. Concerning vascular complications, more investigations are needed.9 Considering the contradictory results in previous studies, the advantages and disadvantages of the two methods, which are sometimes irreparable for patients, nurses’ increased workload, and the higher costs of the healthcare system, this study was conducted to determine and compare vascular complications related to arterial sheath removal using ClampEase device and manual compression in patients undergoing angiography.
Materials and Methods
This experimental clinical trial was conducted on non-blinded patients undergoing angiography through the femoral artery. Vascular complications after arterial sheath removal were compared in manual compression and ClampEase Model C750 methods. In the manual method, constant pressure was applied to the sheath’s removal site after removing the sheath until homeostasis was achieved. While in the ClampEase device method, after fixing the device under the patient and placing the clamp 2 cm above the catheter insertion site, the sheath was removed, and the device clamp was fixed on the catheter insertion site until hemostasis was achieved. After obtaining written and oral consent from patients, the subject size was calculated 91 patients according to the inclusion criteria, using statistical methods for determining the subject size, and consulting with a statistician (Z1=0.95 in the two-domain test is equal to 1.96, d=0.12, P2 = 0.28, P1=0.16).
Subjects were selected through the convenient sampling method and were randomly allocated to two groups. Random allocation of subjects into two groups as patients with even file numbers in the manual compression group and patients with odd file numbers in the ClampEase device group. Shahid Chamran heart hospital in Isfahan was selected as the main setting for selecting subjects and conducting the study. Inclusion criteria included the international normalized ratio (INR) less than 1.8, using the minimum heparin dose (<5000 units) during angiography,10 no previous hematoma or ecchymosis during the angiography in cath lab or recent hospitalization,11 no osteoporosis, angiography through the femoral artery, and no history of femoral and pelvic surgeries, including replacement of the femoral head and pelvic fractures.12 Sampling began on October 31, 2021 and continued until December 24, 2021 and during the sampling process, there was no subject attrition. In this study, two tools were used to examine the variables: a transparent flexible ruler – a standard and straightforward method for measuring the area of hematoma and ecchymosis and the digital scale model DM3. The length, width, and the area of the raised site, which felt firm while touching by a hand, were calculated using the ruler. Its validity and reliability were determined using another standard ruler.13This ruler was also used to measure the area of skin ecchymosis. Using this tool, the area of ecchymosis (skin discoloration following subcutaneous hemorrhage), which was soft with no firmness, was calculated. The second tool was the digital scale model DM3, which was used to weigh blood-stained gases in patients in case of hemorrhage. This scale measures the volume of blood loss with 95% confidence interval (CI) and α=0.05. The validity and reliability of this tool were evaluated with a standard calibrated scale. The incidence of each of the mentioned complications at each stage was included in the questionnaire in full detail (volume, time, extent, and area). The questionnaire consisted of two sections. The first section was related to demographic characteristics, medical history, and previous illnesses. The second section, which included 20 items, was related to arterial sheath removal and associated complications observed since the sheath removal moment to 24 hours later.
After recruiting the subjects, the questions of the questionnaire, including demographic information, age, gender, marital status, education, height and weight, body mass index, history of hypertension, history of high cholesterol, history of smoking, and diabetes, were asked and included in the questionnaire. After providing sufficient and straightforward explanations to the clients about implementation and the vascular complications related to the sheath removal (hemorrhage, hematoma, and ecchymosis), the patient was monitored for heart rate, respiratory rate, and blood pressure. Afterward, the researcher removed the arterial sheath under standard sterile conditions using mechanical and manual methods. The patient was monitored for hemorrhage, hematoma, and ecchymosis totally in 10 steps, 15, 30, and 45 minutes, and also 1 hour, 2 hours, 4 hours, 8 hours, and 24 hours after the sheath removal. In case of vascular complications, its volume and area were calculated using the mentioned tools and recorded in a questionnaire. Ethical considerations of this study included: providing the study subjects with explanations on the confidentiality of information and data and their participation with full consent. Informed and written consent was obtained from the participants. The results of the study were provided to participants if desired. They also had the right to withdraw from the study in case of unwillingness to continue cooperation. The principle of responsible referencing was observed. To analyze the data and investigate the correlation, statistical tests (independent subject t test and chi-square) and linear and logistic regression were used, respectively, using SPSS software version 13.
Results
A total of 92 subjects participated in the study (ClampEase device group: 46 patients, manual compression group: 46 patients)(Figure 1). The patients in both groups were similar in terms of demographic characteristics and medical history (gender, education, marital status, history of smoking, and history of diabetes) (Table 1).
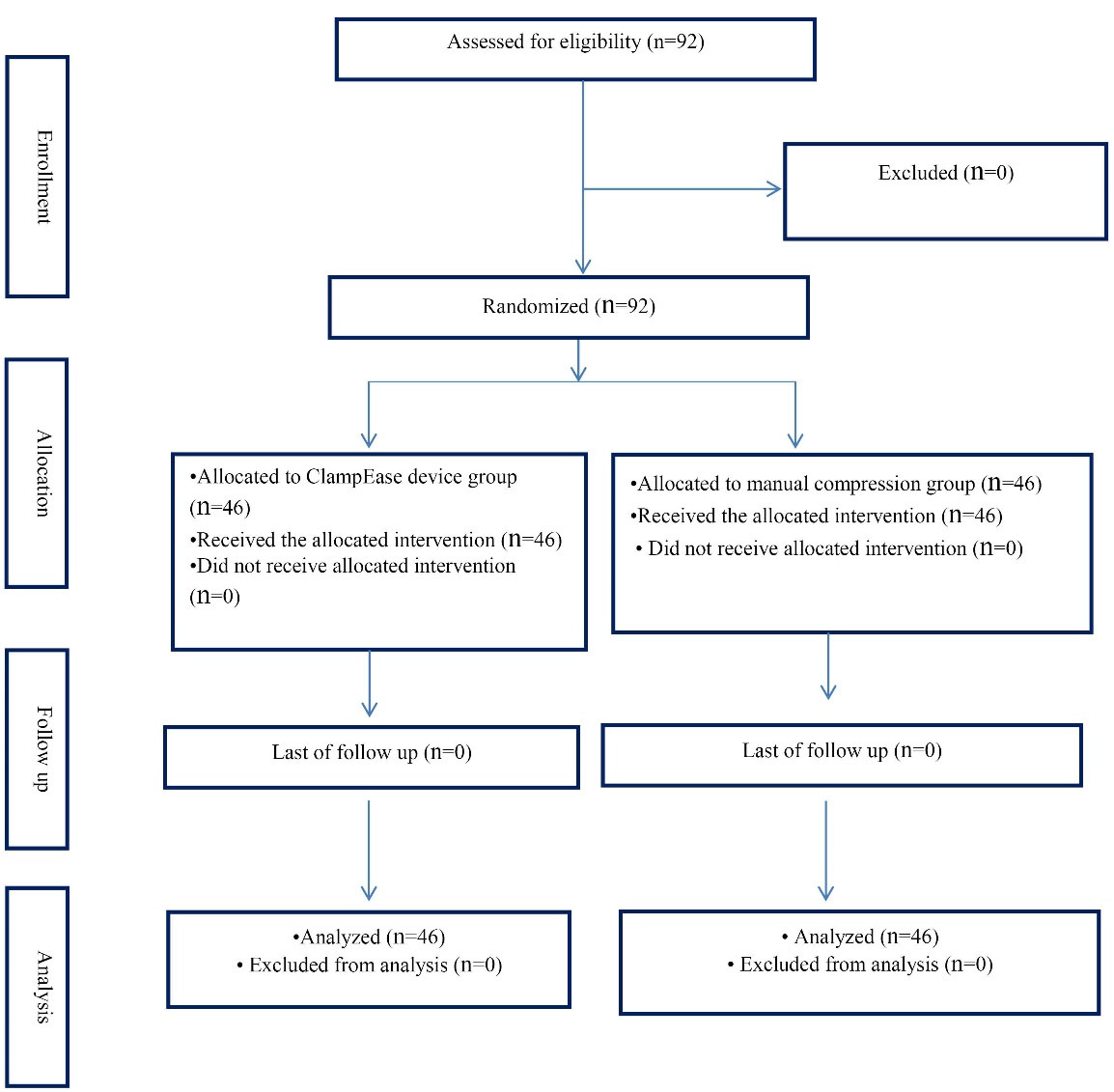
Figure 1.
Flow chart of the study
.
Flow chart of the study
Table 1.
Frequency distribution of studied subjects
|
Variable
|
Manual
|
ClampEase
|
|
No. (%)
|
No. (%)
|
| Gender |
|
|
| Male |
22 (47.8) |
26 (56.5) |
| Female |
24 (52.2) |
20 (43.5) |
| Education |
|
|
| Diploma and less |
39(84.8) |
34 (73.9) |
| Bachelor's degree and higher |
7(15.2) |
12 (26.1) |
| Marital status |
|
|
| Married |
37 (80.4) |
36 (78.3) |
| Single |
9 (19.6) |
10 (21.7) |
| History of smoking |
|
|
| Yes |
15 (32.6) |
21 (45.7) |
| No |
31 (67.4) |
25 (54.3) |
| History of diabetes |
|
|
| Yes |
16 (34.8) |
17 (37) |
| No |
30 (65.2) |
29 (63) |
Chi-square test did not show a significant difference between the two groups of manual and ClampEase in terms of age, gender, marital status, education, history of smoking, history of diabetes, and history of recent angiography. In other words, the two groups were homogeneous. As can be seen in Table 2, the results of the Chi-square test showed a significant difference between the mean of the time of hemostasis, frequency of hemorrhage, frequency of hematoma, and frequency of ecchymosis in the manual method and the ClampEase method considering P < 0.05. The results showed that using the ClampEase device was associated with fewer vascular complications than the manual method.
Table 2.
The relative frequency of hemorrhage, hematoma, and ecchymosis in study subjects of the two manual and ClampEase device groups
|
Variable
|
Manual (n=46)
|
ClampEase (n=45)
|
P
value
a
|
|
No. (%)
|
No. (%)
|
| Homeostasis time (min) |
|
|
0.03* |
| 20 |
44 (97.8) |
38 (82.6) |
|
| 40 |
1 (2.2) |
8 (17.4) |
|
| Frequency of hemorrhage |
|
|
0.01* |
| Hemorrhage |
4(8.7) |
14 (30.4) |
|
| Frequency of hematoma |
|
|
0.04* |
| Hematoma |
5 (10.9) |
13 (28.2) |
|
| Frequency of ecchymosis |
|
|
0.02* |
| Ecchymosis |
6 (13) |
15 (32.6) |
|
aChi-square; *Statistically significant.
As shown in Table 3, there was a difference between the mean volume of blood loss in the ClampEase device and the manual methods. In the ClampEase device method, less volume of blood loss was observed. According to the Student’s t test results (-2.986) and P<0.05, this difference was significant. Regarding the mean area of hematoma, a difference was observed between the ClampEase device and the manual methods, as in the former method, the average area of the hematoma was smaller than the latter method. According to the Student’s t test results (-2.445) and P<0.05, this difference in the mean area of the hematoma was significant in the two methods. Furthermore, there was a difference between the mean area of ecchymosis in the manual and the ClampEase methods regarding ecchymosis. In the ClampEase method, the smaller mean area of the ecchymosis was observed. According to the Student’s t test result (-2.518) and P < 0.05, this difference in the mean ecchymosis area in the two methods was significant.
Table 3.
Comparison of hemorrhage volume, hematoma area, and ecchymosis area of the study subjects in the two manual and ClampEase device groups
|
Variable
|
Mean (SD)
|
Mean difference
|
P
value
a
|
| Hemorrhage volume (mL) |
|
57.82 |
0.006* |
| ClampEase |
9.57 (7.38) |
| Manual |
67.39 (39.5) |
| Hematoma area (cm) |
|
2.94 |
0.02* |
| ClampEase |
0.91 (.49) |
| Manual |
3.85 (2.86) |
| Ecumenical area (cm) |
|
5.1 |
0.01* |
| ClampEase |
2.29 (1.5) |
| Manual |
7.39 (6.7) |
a
t test, *Statistically significant.
Discussion
This study aimed to determine and compare vascular complications associated with arterial sheath removal using ClampEase device and manual compression in patients undergoing angiography and introduce an appropriate and practical method based on findings to remove arterial sheath with minimal vascular complications. This study results showed that using the ClampEase device in patients after angiography was a safe method that was accompanied by fewer vascular complications following arterial sheath removal compared to the manual compression method. This study also showed that the ClampEase device method was associated with less time to achieve homeostasis after arterial sheath removal, leading to the patient’s comfort, faster recovery, and better acceptance. In this regard, to date, various studies have been carried out to investigate the safety of vascular closure devices. A meta-analysis was conducted by Dahal et al to evaluate and compare manual compression method and vascular closure devices. This study examined and analyzed a total of 18 802 patients undergoing femoral artery angiography. The results showed that manual compression increased the time to achieve homeostasis and the risk of hematoma compared to vascular closure devices.14
The present study results likewise showed that the manual compression method was associated with a higher incidence of hematoma and the greater mean area of hematoma that required more time to achieve homeostasis. In this regard, a meta-analysis was conducted by Biancari et al with the aim of evaluating the safety and efficacy of vascular closure devices on 7528 patients following angiography. The results showed that using these devices causes homeostasis to be achieved in a shorter period of time that was in line with the present study and supports our findings; however, further studies are needed to obtain more definite results.8 In this regard, a review was conducted by Cox et al in 2015 on 34 randomized controlled studies including all available RCTs up to 2015 that had compared vascular closure devices with manual compression.9 The mentioned study results showed that the vascular closure devices needed a shorter time for achieving homeostasis, bed rest, and discharge compared to patients who used the manual method. There is a need for further investigation in the field of vascular complications. Accordingly, the results obtained in this review supported the results of the present study.15 As a result, using the ClampEase device method in patients can help shorten the hospital stay length and accelerate getting out of bed. Beneficial and valuable studies have been carried out to evaluate and compare the arterial sheath removal methods after angiography. One of these studies is a systematic review conducted by Noori to systematically evaluate vascular closure devices approved by the Food and Drug Administration and compare them with the manual compression method in patients undergoing angiography through the femoral artery. This study, carried out through searching databases (MEDLINE and PubMed), investigated a total of 14 746 patients undergoing angiography. The results showed that vascular closure devices provided the maximum patient comfort and satisfaction level and required a shorter time to achieve homeostasis after sheath removal. Patients suffer less pain when using these devices than the manual compression method, which provides more comfort and convenience. This systematic study also showed that vascular closure devices were associated with fewer vascular complications and less hemorrhage after arterial sheath removal,16 which was consistent with the present study results.
Conclusion
The findings of this study showed that using the ClampEase device method in patients after angiography was a safe method with fewer vascular complications after arterial sheath removal compared to the manual compression method. This finding can help reduce hospital costs and hospital stay length. As the study results showed, the ClampEase device method was associated with less time to achieve homeostasis after arterial sheath removal, leading to patient comfort, faster recovery.
It is suggested that in the next research, other complications after the removal of the arterial sheath, including pain, should be investigated and researched.
Acknowledgments
The present study is based on a master thesis in nursing.The researchers are extremely grateful to the Vice-Chancellor for Research of Isfahan University of Medical Sciences, the staff of Shahid Chamran Hospital of Isfahan, and all who helped in this research.
COI-statement
The authors declared no conflict of interest in this study.
Data Availability Statement
The datasets are available from the corresponding author on reasonable request.
Ethical Approval
This research has been approved by the Ethics Committee of Isfahan University of Medical Sciences (IR.MUI.NUREMA.REC.1400.177).
Research Highlights
What is the current knowledge?
-
Vascular complications including hemorrhage, hematoma, and ecchymosis are the most common complications after arterial sheath removal in patients undergoing coronary angiography.
-
Manual compression and The ClampEase are the most widely used method of inducing homeostasis in patients undergoing coronary angiography.
What is new here?
-
The ClampEase device method in patients after angiography was a safe method with fewer vascular complications after arterial sheath removal compared to the manual compression method.
-
In the ClampEase device method, less volume of blood loss was observed, the average area of the hematoma was smaller and the smaller area of the ecchymosis was observed.
References
- Libby P. Braunwald’s Heart Disease. 12th ed. Netherlands: Elsevier; 2021.
- Kennedy SA, Rajan DK, Bassett P, Tan KT, Jaberi A, Mafeld S. Complication rates associated with antegrade use of vascular closure devices: a systematic review and pooled analysis. J Vasc Surg 2021; 73(2): 722-30.e1. 10.1016/j.jvs.2020.08.133
- Sedghi Sabet M, Benvan G, Baghaie M, Atrkar-Roshan Z, Khalili M. Vascular complications and its related factors after coronary angiography. Iran Journal of Nursing 2015; 27(92):13-22. doi: 10.29252/ijn.27.92.13 [Crossref] [ Google Scholar]
- Ruiz AM, Sheharyar A, Ortega-Gutierrez S. Arterial access and intermediate catheters: procedural and technical considerations. In: Samaniego EA, Hasan D, eds. Acute Stroke Management in the Era of Thrombectomy. Cham: Springer; 2019. p. 47-60. 10.1007/978-3-030-17535-1_5
- Masoomi R, Khera S. Vascular closure devices and complications. In: Kini A, Sharma SK, eds. Practical Manual of Interventional Cardiology. Cham: Springer; 2021. p. 167-86. 10.1007/978-3-030-68538-6_13
- Bhogal S, Waksman R. Vascular closure: the ABC’s. Curr Cardiol Rep 2022; 24(4):355-64. doi: 10.1007/s11886-022-01654-z [Crossref] [ Google Scholar]
- Huang PH, Hassan AKM, Resnic FS. Manual, mechanical, and device hemostasis. In: Lanzer P, ed. Textbook of Catheter-Based Cardiovascular Interventions: A Knowledge-Based Approach. Cham: Springer; 2018. p. 435-63. 10.1007/978-3-319-55994-0_28
- Biancari F, D’Andrea V, Di Marco C, Savino G, Tiozzo V, Catania A. Meta-analysis of randomized trials on the efficacy of vascular closure devices after diagnostic angiography and angioplasty. Am Heart J 2010; 159(4):518-531. doi: 10.1016/j.ahj.2009.12.027 [Crossref] [ Google Scholar]
- Cox T, Blair L, Huntington C, Lincourt A, Sing R, Heniford BT. Systematic review of randomized controlled trials comparing manual compression to vascular closure devices for diagnostic and therapeutic arterial procedures. Surg Technol Int 2015; 27:32-44. [ Google Scholar]
- Ho HH, Jafary FH, Ong PJ. Radial artery spasm during transradial cardiac catheterization and percutaneous coronary intervention: incidence, predisposing factors, prevention, and management. Cardiovasc Revasc Med 2012; 13(3):193-5. doi: 10.1016/j.carrev.2011.11.003 [Crossref] [ Google Scholar]
- Pieper CC, Thomas D, Nadal J, Willinek WA, Schild HH, Meyer C. Patient satisfaction after femoral arterial access site closure using the ExoSeal® vascular closure device compared to manual compression: a prospective intra-individual comparative study. Cardiovasc Intervent Radiol 2016; 39(1):21-7. doi: 10.1007/s00270-015-1204-2 [Crossref] [ Google Scholar]
- Klein-Wiele O, Baliota M, Kara K, Käunicke M, Schäfer H, Garbrecht M. Klein-Wiele O, Baliota M, Kara K, Käunicke M, Schäfer H, Garbrecht M, et alSafety and efficacy of clip-based vssuture mediated vascular closure for femoral access hemostasis: a prospective randomized single center study comparing the StarClose and the ProGlide device. Catheter Cardiovasc Interv 2018; 91(3):402-7. doi: 10.1002/ccd.27116 [Crossref] [ Google Scholar]
- Robertson L, Andras A, Colgan F, Jackson R. Vascular closure devices for femoral arterial puncture site haemostasis. Cochrane Database Syst Rev 2016; 3(3):CD009541. doi: 10.1002/14651858.CD009541.pub2 [Crossref] [ Google Scholar]
- Dahal K, Rijal J, Shahukhal R, Sharma S, Watti H, Azrin M. Comparison of manual compression and vascular hemostasis devices after coronary angiography or percutaneous coronary intervention through femoral artery access: a meta-analysis of randomized controlled trials. Cardiovasc Revasc Med 2018; 19(2):151-62. doi: 10.1016/j.carrev.2017.08.009 [Crossref] [ Google Scholar]
- Mohanty S, Trivedi C, Beheiry S, Al-Ahmad A, Horton R, Della Rocca DG. Mohanty S, Trivedi C, Beheiry S, Al-Ahmad A, Horton R, Della Rocca DG, et alVenous access-site closure with vascular closure device vsmanual compression in patients undergoing catheter ablation or left atrial appendage occlusion under uninterrupted anticoagulation: a multicentre experience on efficacy and complications. Europace 2019; 21(7):1048-54. doi: 10.1093/europace/euz004 [Crossref] [ Google Scholar]
- Noori VJ, Eldrup-Jørgensen J. A systematic review of vascular closure devices for femoral artery puncture sites. J Vasc Surg 2018; 68(3):887-99. doi: 10.1016/j.jvs.2018.05.019 [Crossref] [ Google Scholar]