Journal of caring sciences. 12(1):14-24.
doi: 10.34172/jcs.2023.31750
Systematic Review
The Impact of Early Enteral Nutrition on Post-operative Hospital Stay and Complications in Infants Undergoing Congenital Cardiac Surgery: A Systematic Review and Meta-analysis
Sanjay Dhiraaj Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Validation, Writing - Original Draft, Writing – review & editing, 1 
Latha Thimmappa Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing - Original Draft, 2 
Alwin Issac Conceptualization, Writing – review & editing, 3 
Kurvatteppa Halemani Conceptualization, Data curation, Methodology, Writing - Original Draft, 4, * 
Prabhaker Mishra Formal analysis, Supervision, Visualization, 5 
Anusha Mavinatop Validation, 6
Author information:
1Department of Anesthesiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
2College of Nursing, All India Institute of Medical Sciences, Kalyani, West Bengal, India
3College of Nursing, All India Institute of Medical Sciences, Bhuvneshwar, Odisha, India
4College of Nursing, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
5Department of Bio-statistics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
6Department of Nutrition & Dietician, JSS Academy of Higher Education, Mysore, Karnataka, India
Abstract
Introduction: The congenital cardiac diseases (CHDs) are the leading cause of death in children. The CHDs detection and management have greatly improved over the past few decades. This review aimed to assess the effectiveness of early enteral nutrition (EEN) on postoperative outcomes in infants undergoing congenital cardiac surgery.
Methods: Electronic databases PubMed, Clinical Key, UpToDate, the Cochrane Library, and Google Scholar were searched for studies published in the English language, between 2004 and 2021. This review carried out based on PRISMA statement and studies qualities assessed using "Downs and Black score". Hospital stay, intensive care unit (ICU) stay, mechanical ventilation support, aortic cross clamping and cardiopulmonary bypass were as primary outcomes. Similarly infections, vomiting and mortality were as secondary outcomes of included studies.
Results: This review consists of 887 infants from 10 studies. Of these, 470 infants were assigned to the intervention group and 417 to the control group. The post-operative hospital stay shorted in the EEN group than the control group (SMD=-0.63, 95% CI: -1.03 to -0.22, P=0.0, I2=87%). Similarly, EEN group lessen the ICU stay (SMD=-0.15, 95% CI: -0.42, 0.11, P=0.0, I2=71%), mechanical ventilation support (SMD=-0.31, 95% CI: -0.51, -08, P=0.08, I2=47%), aortic cross clamping (SMD=-0.92, 95% CI: -0.31, 2.4, P=0.00, I2=96%), and cardiopulmonary bypass (SMD=-0.0, 95% CI: -0.42 to 43, P=0.00, I2=71%). Secondary postoperative complications such as infections (RR=0.68, 95% CI: 0.43 to 1.08, P=0.40, I2=3%). vomiting (RR=1.47, 95% CI: 0.80 to 2.69, P=0.90, I2=0%) and postoperative mortality (RR=0.42, 95% CI: 0.03 to 5.82, P=0.00: I2=80%) significantly reduced. Conclusion: Postoperative outcomes were improved in the intervention group compared to the control group, including shorter hospital stays, ICU stays, mechanical ventilation, and less postoperative complications.
Keywords: Infant, Early enteral nutrition (EEN), Post-operative period, Congenital heart diseases, Congenital abnormalities
Copyright and License Information
© 2023 The Author(s).
. This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Introduction
Congenital cardiac diseases (CHDs) are a common birth defect that is one of the leading causes of death in children. Globally 6% of neonates are born with a congenital anomaly, which result in 2.4 million newborn deaths. Another 1.7 million children between one month and five years succumb to birth defects,1 of which 1.2 million children per year reported congenital cardiac malformation. However neonates who born with cardiac defects may have longer and healthy lives. Conventionally, number of death due to congenital cardiac defects drastically declined from 398 580 (268 422–506 469) to 261 247 (216 567–308 159) 34.5% between 1990 and 2017.2,3 Incidence of CHDs in India ranged from 8-12 per 1000 live births. Approximately Every year, 0.2 million neonates are born with congenital heart disease. Of these, 20% of children required immediate interventions.4-6
The early detection and management of CHDs increased over the period of time. The survive rate of the newborn after congenital cardiac surgery improved from 67.4% to 82.5% in 1979-2005.7 However, evidence based intervention and modern technologies are essential for reducing CHDs related mortality.
Patients who underwent cardiac surgery are not allowed to oral feeding until their bowel activity returned. Reestablishing feeding after surgery is a challenging and positive sign of the postoperative outcome, especially for children and those who are susceptible to nutritional deficiencies.8 Therefore, it is crucial for children who underwent congenital surgeries to have enough electrolytes and nutrients for post-operative recovery.9 Consequently, early enteral nutrition (EEN) reduced the length of hospital stay and post-operative complications following congenital cardiac surgery.10 There are number of studies available for management of congenital heart diseases. Nevertheless, only a few studies reported contradictory data regarding the use of EEN after congenital heart surgery.11,12
Children who underwent cardiac surgery need the increased continue nutrition supplementation to meet their metabolic demands. Therefore this systematic review and meta-analysis were conducted to evaluate the efficacy of EEN on postoperative outcomes of infants undergoing congenital cardiac surgery. Authors have synthesized data from various research designs of the study attributed to scarcity of randomized controlled trials (RCTs) introducing moderate to high heterogeneity. Therefore we conducted this systematic review and meta-analysis of quantitative studies to analyze the efficacy of EEN on post-operative outcomes of children undergoing congenital cardiac surgery.
Materials and Methods
This systematic review and meta-analysis was registered in PROSPERO (National Institute for Health Research-International prospective register of systematic reviews) and is available online CRD42022329349. The aim of this systematic review and meta-analysis was to appraise the evidence on the EEN on post-operative outcome of neonates undergoing congenital cardiac surgery. This systematic review and meta-analysis was carried out based on Cochrane collaboration guidelines13 and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.14 The search strategy was developed using the keywords of population or patient, intervention, comparator or control, and outcome (PICO). Two authors (KH, SD) independently searched the databases; PubMed, Clinical Key, UpToDate, CINAHL (Cumulative Index to Nursing and Allied Health Literature), the Cochrane Library, and Google Scholar with filters in the study period. Present review was considered experimental and non-experimental studies for evaluating the efficacy of the EEN on postoperative outcomes among the infants undergoing congenital cardiac surgery.
MeSH (Medical Subject Headings) terms used during the online search were: (neonate or newborn or infant) and (early nutrition or enteral nutrition or nutrition supplementation or early enteral nutrition) and (hospital stay or ICU stay) and (cardiac surgery or congenital cardiac surgery or congenital cardiac repair). Further a manual search of the citations and references of the primary studies were carried out. Duplicate records were removed after screening the titles and abstracts and the remaining original full articles were screened to assess the inclusion criteria.
Along with RCTs we considered non-randomized control designs, and observational studies published in English language. All primary studies reported early enteral feed (oral or nasogastric feed) or supplementary nutrition or additional calories/energy feed given in experimental groups.
Search scheme retrieved 36 652 studies from various databases and 3 studies were retrieved from printed materials. During the initial screening, 1750 duplicate articles were removed. The remaining 34 905 articles were screened. Further 34 761 articles were removed after reading through the titles and abstract, as they didn’t meet the predetermined inclusion criteria of the review. The remaining 128 articles were read and screened for eligibility, of which 117 articles were removed. The reason for excluding the articles: articles which did not report sample size and primary outcomes, statistical information were lacking. Finally, 11 articles were selected for narrative synthesis and meta-analysis. The study selection process is depicted in Figure 1.
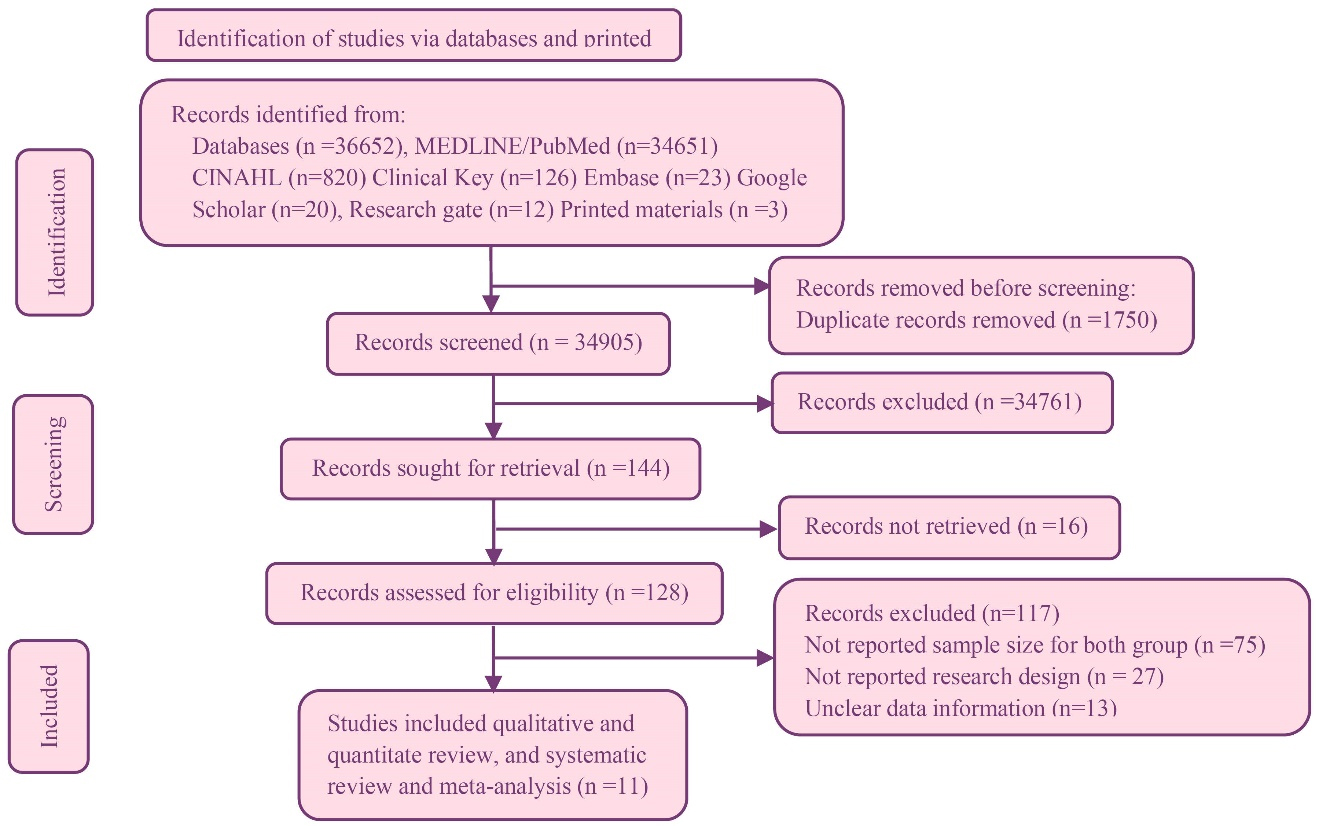
Figure 1.
Prisma flow digram of study selection
.
Prisma flow digram of study selection
Participants of this review were postoperative infants underwent congenital cardiac surgery.
Infants in the experimental group received the EEN, whereas those in the control group were given expressed breast milk or supplementary feed in accordance to the hospital norms.
The nature of subjects,15 authors had failed to report the specific nutritional supplementation and volume. However, non-invasive interventions like nutrition therapy are the vital elements in enhancing feeding tolerance and post-operative outcomes in growing neonates. Intervention group received enriched energy (EE) or high calories or supplementary nutrition16-21 and Human Milk Fortifier (HMF).22,23 Every two to three hours, a calculated postoperative protein energy feed was administered.24-26 On the other hand, control group received the nutrient as per agency protocol (Table 1).
Table 1.
Summary of the included studies
|
Author, year, Country
|
Sample
size
|
Research design
|
Intervention
|
Inclusion criteria
|
Exclusion criteria
|
Results
|
Outcome
|
Ehrmann et al,16 2017
USA |
T-69
AC-49
ANC-20 |
Retrospective single center study design |
Neonates receive intervention by trained therapist. Critically ill infants given special consideration after medically fit through continuous NG feed after surgery. All oral feed volume assessed by the feeding therapist through evidenced-based oral feeding guideline. |
All neonates less than 3 months admitted for their first cardiac surgery between January 1, 2015, and December 31, 2016 |
Neonates not admitted unable to meet key decision algorithm [sentinel FRA] |
The ACL had longer hospital stay (34 versus 25 days; P=0.01) than AC. Among GT recipients, noncomplainers waited 6 additional days for a GT compared with compliers (P≤0.001). |
AC significance after congenital cardiac surgery. Feeding skills heighten the FRAs. |
Yoshimura et al,17 2015
Japan |
T-109
Post group-47
Pre group-62 |
Prospective single center
compared with historical cases research study |
Post group EN was estimated by therapist, using standard guidelines (1 to 5 months: 55 kcal/kg/d; 6 to 12 months: 50 kcal/kg/d; 1 to 2 years: 45 kcal/kg/d; >3 years: 40 kcal/kg/d). Milk (<12 months) or formula (>1 year) was given through GT. The initial dose of EN was set at 10% of the target daily dose gradually increased. |
Children admitted to the ICU and stayed more than 72 hours were enrolled in this study (post group). Pre groups were children admitted in ICU between June 2010 to August 2012; |
Less than one month, gastrostomy tube, NEC hemodynamically unstable, supported on extracorporeal membrane oxygenation, or gastrointestinal bleeding. |
Post-operative complication like vomiting significantly decreased in post group than in the pre group (36.2% versus 58.0%, P=0.038). |
The post group significantly reduced the vomiting, NEC and post-surgical complication. |
| Du et al18 2021 China |
T-98
24H-66
6H -32 |
Retrospective single center
study |
Thirty-two neonates received EN within 6 hours of surgery, while 66 neonates administered after 24 hours.
Similarly post CHDs surgery neonates admitted in CICU of Guangzhou Women and Children’s Medical Center between Jan 2016 to Dec 2017 were introduced EN within 6 hours. |
The inclusion criteria were neonates; complex CHDs children with risk adjustment for congenital heart surgery. |
Premature infants; coarctation of the aortic or left ventricular outflow GI ischemia before surgery. Children undergoing hemodialysis; children receiving extracorporeal membrane oxygenation; and children with incomplete data. |
The incidence of feeding intolerance was 56.3% in 24-hour group and 39.4%, respectively (P=0.116). As compared to 24-hour
Group, prealbumin and retinol binding protein levels were higher (160.7±64.3 vs 135.2±28.9 mg/L, P=0.043 for prealbumin; 30.7±17.7 vs 23.0±14.1 g/L, P = 0.054 for retinol-binding protein). The duration of CICU stay (9.4±4.5 vs 13.3±10.4 days, P=0.049) and hospital stay (11.6±3.0 vs 15.8±10.3 days, P=0.028) were shorter in 6-hour group. |
Early postoperative EN can shorten the time of postoperative intestinal paralysis, improve the microcirculation of liver and intestinal mucosa, and prevent the imbalance of intestinal flora, so it may better regulate gastrointestinal function, promote the recovery of gastrointestinal function, and reduce the incidence of feeding intolerance. |
Scheeffer et al,19 2020,
Brazil |
T-59
E-29
C-30 |
Two arm Single center blinded RCT |
EE formula while control group received normal caloric hydrolyzed formula. |
Babies undergoing heart surgery in a tertiary hospital in southern Brazil from March 2017 to December 2017. |
Cow’s milk protein allergy. |
GI side effects more significant in control group than the experimental group. However diarrhea often reported in experimental group. |
Use of EE formula feed more effective in intervention group in post operatively, need of hospitalization and antibiotics significantly reduced in experimental group. |
Sahu et al,202016,
India |
T-50
E-25
C-25 |
Single center and blinded RCT |
The nutrition requirement of babies was calculated using past 24 hours feed volume and child cardiac functions.
Both received EBM (0.65 kcal/mL), while children in intervention group received supplementary formula (0.91 kcal/mL). |
The CHDs babies’ age less than 6 months required elective surgery.
And was availability of mother’s milk. |
Babies born before gestational age. Multi organ congenital, anomalies emergency operations, and closed heart surgery. |
Need for mechanical ventilator between control and intervention group (153.6±149.0 vs. 123.2±107.0 hours, P=0.20). Similarly, infants in the intervention group spend less time in the ICU (11.0±6.1 days) and hospital stay (14.1±7.0 days) then infants in the control group, ICU (13.2±8.9 days) & hospital (16.5±9.8 days). The infection rate (3/25; 5/25) and mortality rate (1/25; 2/25) were lower in the intervention. |
EBM and EEN reduced the hospital stay, ICU stay and mechanical ventilation, rate infections and mortality rate. |
Pillo-Blocka et al,21 2004
Canada |
T-46
E-23
C-23 |
Single center double blinded RCT |
Additional concentration of enteral feeds given in intervention group,
The calculated daily volume of enteral feeds was ordered for each study subject through the hospital’s computerized medical order system. |
The infant under one year old admitted for congenital cardiac surgery. |
All infants with gastrointestinal malformations, preoperative- reflux, or genetic conditions and palliative operations were excluded. |
The energy intake estimated before discharge from hospital. About 98% in intervention and 78% control group meet the energy level. Infants in the intervention group gained weight and shorten the hospital stay. |
Rapid advancement of nutrition decreased the hospitalization and post-operative outcome. |
Chen et al,22 2021
China |
T-244
E-124
C-120 |
Single center RCT |
Intervention group received the high energy nutrition milk powder
(100 kcal/100 mL). Control group received nutrition based on dietician (67–82 kcal/100 mL) until discharge. All nutrients & volume of enteral feed was calculated by chief dietician & surgeon. |
Infants less than 6 months age undergoing congenital heart surgery with mild and moderate or severe malnutrition. |
Patients with genetic diseases, malnourished infants, and parents refused consent. |
Intervention group received high calories than control group (44.5 vs. 34.7; P<0.001). ICU stay, need of mechanical ventilation support and infection rate (P=0.001) were significantly lower in the intervention group than the control group. At 3 months post-surgery, the intervention group reported higher recovery from malnutrition (19.4% vs. 6.5%; P=0.002). |
The early high-energy nutrition in intervention group drastically improved recovery, reduced ICU stay, mechanical ventilator and postoperative infection rates. |
Yu et al,23 2021
China |
T-54
E-27
C-27 |
Single center
RCT |
The intervention group received the
80–100 mL/kg/d. HMF was
produced by Nestlé, Germany. In the beginning, one-quarter of a gram of HMF was added to 25 mL of breast milk (25 ml breast milk: 0.25 g of HMF). HMF increased from 0.2.5 g to 0.5 g to 1g during next 6 days. |
1. Age<4 months; 2.
Availability of mother milk; 3. Good recovery of cardiac and
Circulatory functions after surgery; 4. Stable hemodynamics
and satisfactory correction of intracardiac malformations; and
5. Parents signed informed consent. |
Baby born before completion of gestational age, those babies suffered to pulmonary
Infection and other organ malformations before surgery; emergency surgery. The parents who declined to participate and infants who were fed formula milk. |
Infant in intervention group less ICU stay (5.0±2.1 days) than the control group (5.8±2.9 days). The intervention group's hospital stays were shorter than the control groups. |
Compared with breastfeeding alone, with HMF can improve postoperative
weight gains, reduce the length of stay, and promote infants’ early recovery after
congenital cardiac surgery. |
Kalra et al,24 2018
India |
T-30
E-15
C-15 |
Single center blinded prospective
RCT |
Children were randomly allocated in feed group & NPO group. Feed group received trophic feeds
10-20 mL/kg/d postoperatively.
Increased the feed volume until it reached the desired volume.
Those were in NPO group received the nutrients after extubating. |
All newborns with cyanotic congenital heart disease weighed less than 5 kg. |
Infants admitted for palliative procedures, open chest, requiring ECMO before leaving operating room.
Any associate GI malformation to initiate enteral feed and parent’s denied for assent. |
The time of mechanical
ventilation reduced in the feeds group (58.2±4.71). Similarly, need for ICU stay decreased (179.04±41.28 vs 228.72±85.44 h) than control group. |
Neonates well tolerated for immediate feed following congenital heart surgery.
Moreover, feeds appear to decrease duration of mechanical ventilation and ICU stay. |
Cui et al,25
2018,
China |
T-50
PE-26
S-24 |
Single center double blinded RCT |
For intervention group given PE-formula (2.6 g/100 mL, 100 kcal/100 mL) through nasogastric tube. Similarly, control group (S-group)
administered standard protein and energy formula (1.4
g/100 mL, 67 kcal/100 mL) |
(1) congenital heart surgery, (2) Infants age between 1 month and 3 months
(3) Full term babies. |
(1) Multi organ congenital anomalies (2) application
of parenteral nutrition; (3) correction of simple congenital surgery; (4) combined inherited metabolic diseases; chromosomal liver and kidney. |
Nutrient intakes were significantly higher
in the PE-group after 24 hours and maintained the essential nutrients by the end of 2nd post-operative day. Positive nitrogen balance found in the PE-group. In context, S-group, (control) taken time recovery. Experimental group (PE-group) found positive essential amino acids. |
Infants in PE-group, early administration of PE-formula was as well tolerated than the control group (S-formula group). The PE group makes a substantial effort to maintain all nutrients, including nitrogen balance. |
Liu et al,262021
China |
78
E-39
C-39 |
Single center RCT |
Two groups (A and B) separately received post-operative feed at two intervals for the first 24 hours. Then, gradually increased feed volume. |
Infants that were diagnosed with simple, unrestricted VSDs before or after birth who
underwent surgical repair with cardiopulmonary bypasses
less than 2 months and whose weight
was greater than 3.5 kg. |
Patients with severe liver or renal, patients whose VSDs were combined with digestive tract malformations necrotizing enterocolitis; patients with parents who refused to participate in this study. |
The feeding time for group A was significantly higher than group B (142.5±15.4 vs. 132.0±16.1). Job satisfaction among nurses reduced in group A than group B (101.7±9.8 vs.
108.8±10.1, P=0.005).
Similarly, duration of mechanical ventilation (3.7±1.1 vs. 3.9±1.0 d, P=0.272), ICU stays(4.5±1.1 d vs. 4.7±0.9 d, P=0.451), and hospital stays(13.2±1.4 vs. 3.3±1.0 d, P=0.642)shorten in the intervention group than in the control group, but this was not statistically significant. |
Group A increased the feed tolerance and that impacts job satisfaction of healthcare workers. |
AC, algorithm compliers; ANC, algorithm non-compliers; GI, gastrointestinal; NG, nasogastric tube; NCE, necrotizing enterocolitis; VSD, ventricular septal defect; EN, enteral nutrition; CHDs, congenital heart diseases; EEN, energy enrich nutrition; EBM, express breast milk; FRA, feeding readiness assessment; ICU, intensive care unit; CICU, cardiac intensive care unit; EE, energy enriches; RCT, randomized controlled trial.
The authors have synthesized data from different types and designs of the study attributed to scarcity in the number of RCTs introducing moderate to high heterogeneity in certain outcomes. However, we were able to retrieve additional RCTs and bring forth highest level of evidence on the efficacy of EEN on post-surgery outcomes among children born with CHDs.
Two authors independently extracted the data from the included 10 articles and any disagreement between the first and fourth authors (KH, SD) referred to the second author (LT) and resolved the disagreement. The data extraction process was carried out based on the data extraction form: name of the authors, country, year of publication, study design, type of intervention, time of first feed, inclusion and exclusion criteria, study’s result, and outcome.
The quality of the included studies was assessed using the “Downs and Black score.” The tool contains 27 questions with three major domains namely external validity, internal validity and power. Scores of the Downs and Black scale categorized as < 14 low quality, 15-19 fair quality and 20-25 high-quality articles (Table 2).
Table 2.
uality assessment of included studies (Downs and Black score)
|
No
|
Study name, year& country
|
Score
*
|
| 1 |
Ehrmann et al,16 2017, USA |
20 |
| 2 |
Yoshimura et al,17 2015, Japan |
20 |
| 3 |
Du et al,182021, China |
20 |
| 4 |
Scheeffer et al,19 2020, Brazil |
26 |
| 5 |
Sahu et al,20 2016, India |
25 |
| 6 |
Pillo-Blocka et al,21 2004, Canada |
26 |
| 7 |
Chen et al,22 2021, China |
24 |
| 8 |
Yu et al,23 2021, China |
21 |
| 9 |
Kalra et al,24 2018, India |
25 |
| 10 |
Cui et al,25, 2018, China |
26 |
| 11 |
Liu et al,26 2021, China |
21 |
*<14 poor, 15-19 fair, 20-25 good, 26-28 excellent.
Search keywords were “newborn” “neonates” “infant” “toddler” “early nutrition” “nutrition supplementation” “early enteral nutrition” “hospital stay” “surgery” “congenital cardiac surgery” “congenital cardiac repair”.These keywords were searched using the Boolean operator “AND” and “OR”.
The extracted data from the original studies were subjected to meta-analysis. The standardized mean difference was calculated after adjusting standard deviation. Heterogeneity of studies was reported using I2tool, low heterogeneity was considered for an I2 < 25%, moderate heterogeneity for I2 < 75% and high heterogeneity for I2 > 75%. The effect of heterogeneity reduced using a random-effects model to compute mean differences, and standardized mean differences between experimental and control group at 95% confidence interval (CI).15 Incidence of post congenital cardiac surgical complications were reported using risk ratio (RR) at 95% CI and significance was considered at P < 0.05. The pooled data of included studies were analyzed by RevMan software version 5.3 (Cochrane collaboration, Copenhagen, Denmark).
Results
Data from orginal studies were summarised and displayed in tables and forest plots. There were 887 infants from 11 studies included, with 470 infants in intervention group and 417 in the control group. The sample size of primary studies ranged from 30 to 244, with infants age ranging from one to seven months. In five studies, participants and researchers were kept in the blind.19-21,24,25 Three primary studies were not reported as randomized control trials, but they were well-designed16-18 (Table 1). All included studies for this review were calculated nutrition based on body weight and total nutrition volume consumed in the last 24 hours (Table 1).
The primary outcomes were continuous variables that reported mean and standard deviation (hospital stay, ICU stay, duration of mechanical ventilation, Aortic cross clamp and cardiopulmonary bypass). Among two studies, reported median and interquartile range (IQR).21,22 We manually calculated mean and standard deviation for these two studies using mean (SD) conversion formula. Dichotomous variables considered secondary outcomes and analyzed using RR formula.
The result of the meta-analysis of hospital stay showed that pooled standard mean differences of -0.63 were significantly lower in the intervention group compared to the control group with a considerable level of heterogeneity (I2=87%, P<0.001) (N=857) (SMD=-0.63, 95% CI: -1.04 to -0.22) (Figure 2).16-23,25,26
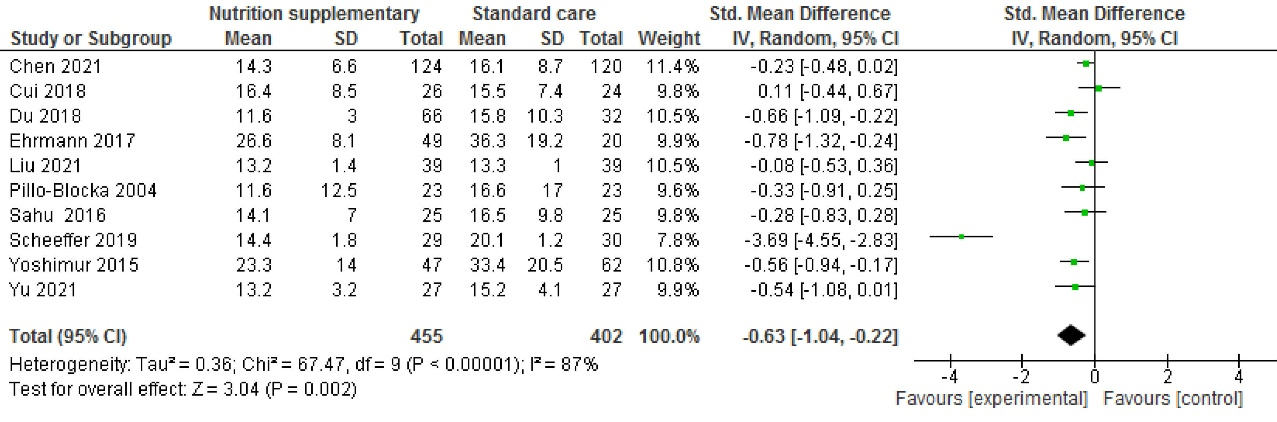
Figure 2.
Length of hospital stay after congenital cardiac surgery (days)
.
Length of hospital stay after congenital cardiac surgery (days)
Similarly, result of the meta-analysis of ICU stay showed that pooled standard mean differences of -0.15 were significantly lower in the intervention group compared to the control group with a considerable level of heterogeneity (I2=71%, P<0.001) (N=887) (SMD = -0.15, 95% CI: -0.42 to 0.11) (Figure 3).16-23,25,26
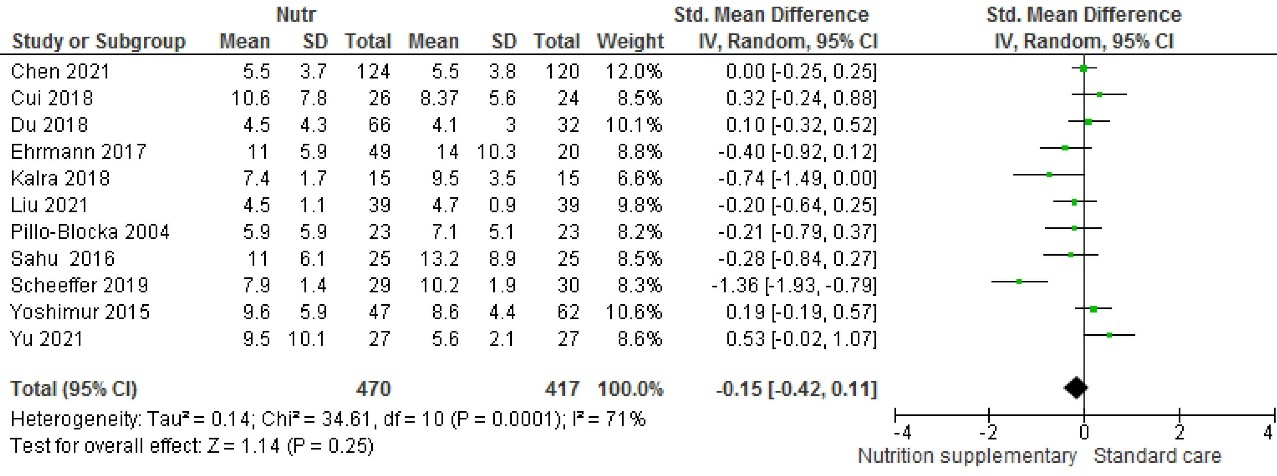
Figure 3.
Length of ICU stay after congenital cardiac Surgery (days)
.
Length of ICU stay after congenital cardiac Surgery (days)
Seven studies reported duration of mechanical ventilation The result of the meta- analysis of duration of mechanical showed that pooled standard mean differences of -0.31 were significantly lower in the intervention group compared to the control group with a considerable level of heterogeneity (I2=47%, P=0.08) (N=648) (SMD=-0.31, 95% CI: -0.54 to -08) (Figure 4).17-23,25,26
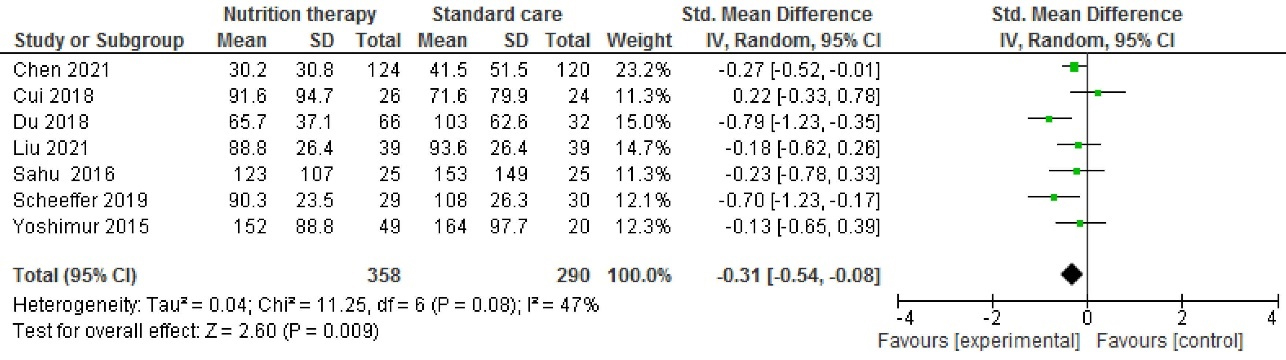
Figure 4.
Duration of mechanical ventilation after congenital cardiac surgery (hours)
.
Duration of mechanical ventilation after congenital cardiac surgery (hours)
Five studies reported the amount of time required for Aortic cross clamp.The result of the meta- analysis of duration of mechanical showed that pooled standard mean differences of 0.92 were significantly higher in the intervention group compared to the control group with a considerable level of heterogeneity (I2=96%, P<0.001) (N=320) (SMD=-0.92, 95% CI: -0.31 to 2.14%) (Figure 5).17,18,20,23,26
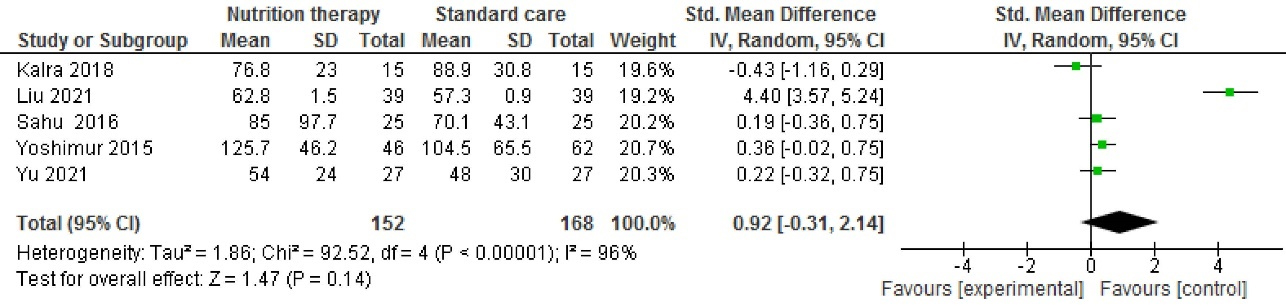
Figure 5.
Time of Aortic cross clamp postopertively (Hours)
.
Time of Aortic cross clamp postopertively (Hours)
Similarly, the result of the meta- analysis of duration of cardiopulmonary bypass that pooled standard mean differences of 0.0 were significantly lower in the intervention group compared to the control group with a considerable level of heterogeneity (I2=71%, P=0.00) (N=21) (SMD=0.0, 95% CI: -0.42 to 43) (Figure 6).17,18,20,23,26
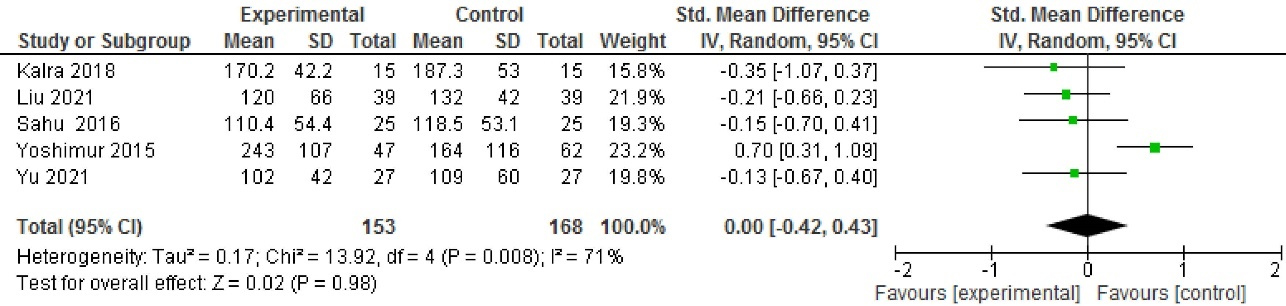
Figure 6.
Time of Cardiopulmonary bypass postoperatively (hours)
.
Time of Cardiopulmonary bypass postoperatively (hours)
Secondary outcomes reported six studies namely post-surgery infections (n=574) (RR=0.68, 95% CI: 0.43 to 1.08, P=0.40, I2=3%),18,20,22,23,25,26 three studies reported vomiting (n=163) (RR=1.47, 95% CI: 0.80 to 2.69, P=0.90, I2=0%)19,23,25 and three studies reported the mortality (n=218) [RR=0.42, 95% CI: 0.03 to 5.82, P<0.001, I2=80],17,19,20 which was addressed by subgroup analysis of overall incidence of surgical complications [RR=0.88, 95% CI: 0.58 to 1.36, P0.08, I2 = 39], subgroup analysis stated [χ2=4.22, df=2, P=0.12] (Figure 7).
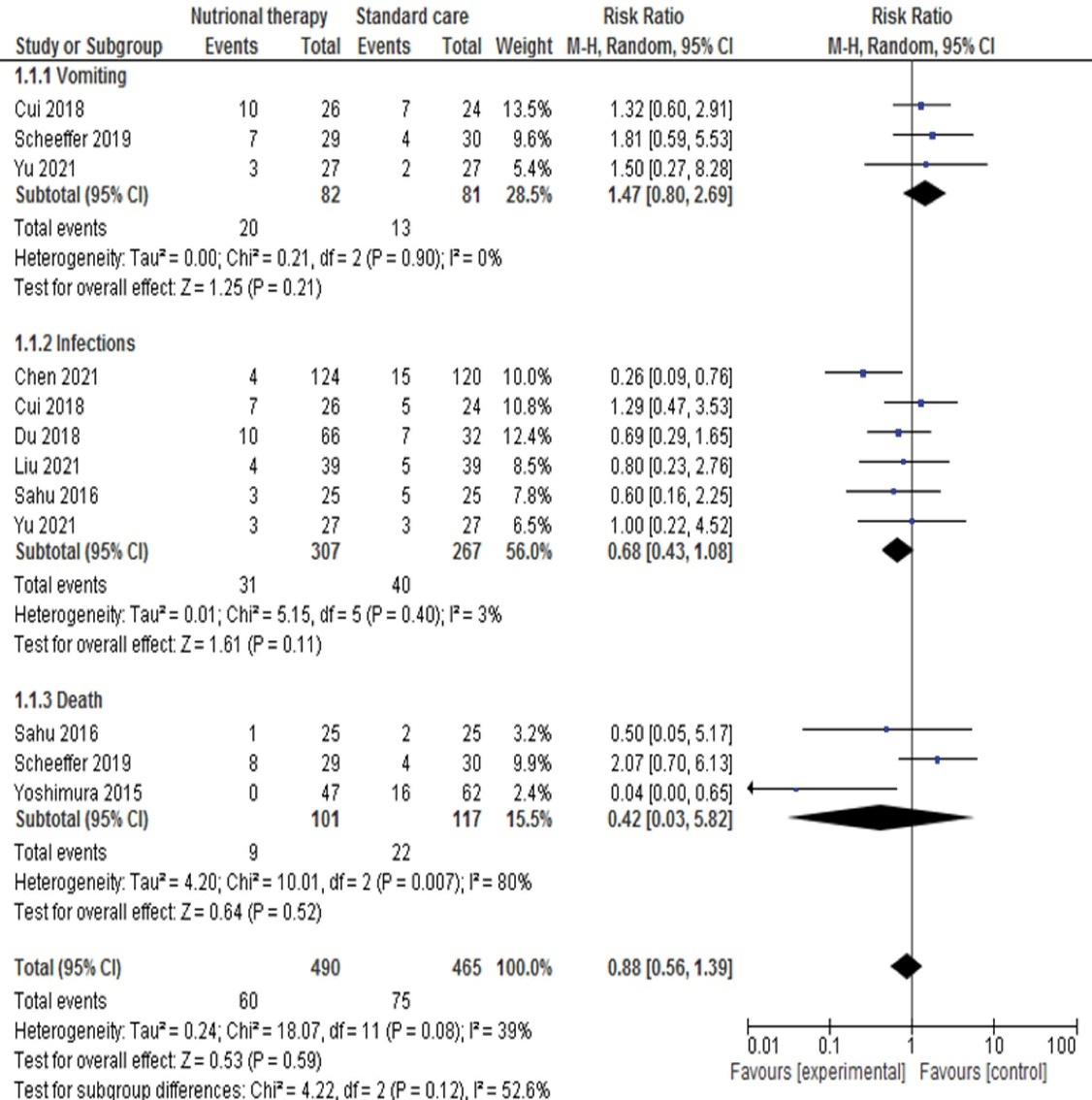
Figure 7.
Postoperative complications
.
Postoperative complications
The number of trials involved in this systematic review and meta-analysis reported publication bias using fixed effect model. In the funnel plots, each dot represents a separate study (Figure 8).
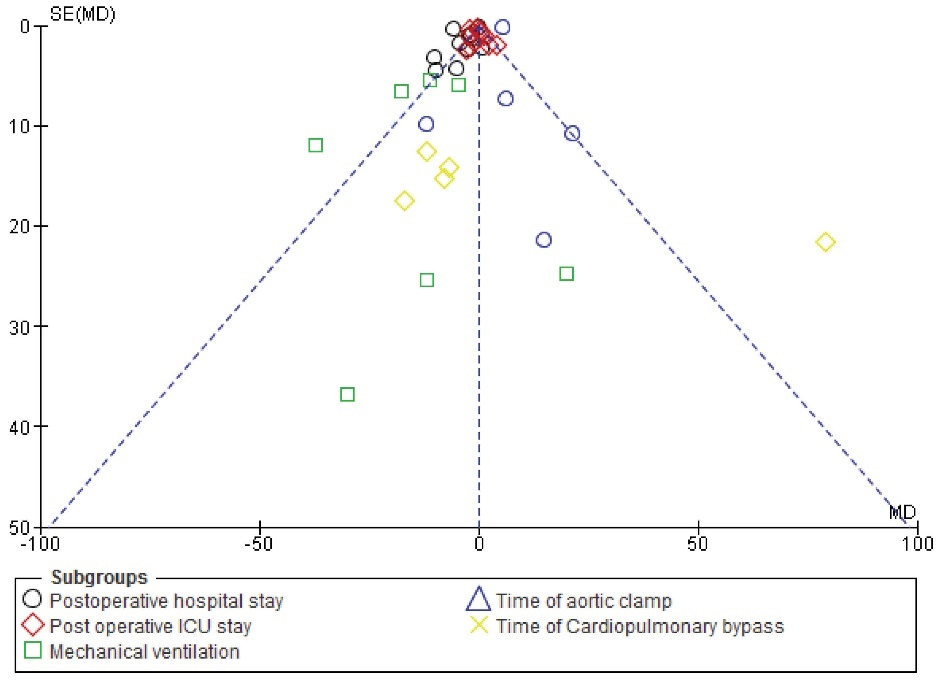
Figure 8.
Publication bias
.
Publication bias
Discussion
This is the first systematic review and meta-analysis assessing the effectiveness of EEN on post-operative outcomes of congenital cardiac surgery in infants. The findings of existing review summarized that early enteral feeding or supplementary nutrition is safe and effective intervention in infants to reduce the post-operative complications, ICU stay and duration of mechanical ventilation.
Little attention is paid to the nutritional management of infants in post-operative nutritional management. There are many extrinsic factors that delay nutritional supplementation in postoperative infants.27 On the other hand, well established clinical guidelines are available for adult but the same protocol does not apply to infants undergoing cardiac surgery.28-30
Nutrition plays a pivotal role in critically ill patients, especially in post-operative patients.31 Other important factors for postoperative management are the timing, type and amount of nutritional supplementation. Parenteral nutrition is a favorable route after surgery, however, because it prevents the aspiration, resulting in vasopressor support in postoperative infants. In this issue, recent studies have suggested that enteral nutrition is the most favorable and immediate replacement of nutrients (24-72 hours) following congenital cardiac surgery.24,32 Nevertheless, It hasn’t been specified how quickly EEN supplementation will progress to postoperative children. Hence this systematic review and meta-analysis was carried out to yield sound evidence that early nutrition feed reduced the post-operative complication following congenital cardiac surgery.
There is evidence available that EEN reduces the length of ICU stays, lessens mechanical ventilation, and decreases hospital expenditure. The findings of our systematic review and meta-analysis are in consensus with previous systematic reviews, which inferred that EEN has positive benefits in comparison to late nutrition administration. Critical illness brings forth numerous hormonal and metabolic derangements, leading to grave micronutrient and macronutrient deficiencies.33 In recent meta-analysis reported that EEN within 48 hours post gastro intestine anastomosis significantly reduced ICU stay, mechanical ventilation supports and reduced the post-operative complications in infants.28 However, the findings of our review, similar to previous systematic review and meta-analysis, have reported on pyloromyotomy34 and abdominal surgery in children,35 with EEN declined hospital stay, ICU stay and postoperative complications in infants.
The key finding of our review is that the total time required for aortic cross clamping is favorable in the intervention group. Similarly, the need for cardio pulmonary support was lower in the intervention group compared to the control group. Apart from this the pooled incidence of the post-operative infections and mortality rates reduced in the intervention group. Although, active involvement of primary caregivers potential impact on post-operative outcome in children.36,37 All primary studies of this review reported that EEN continued to be small, increasing gradually to the target volume within 48-72 hours.
Enteral nutrition is a simple and often substitute marker for post-operative recovery in routine clinical practice.38
However, there is high prevalence of nutritional deficits among neonates especially in pre term and small for gestational babies after congenital cardiac surgery.39 Therefore there is an urgent need for an evidence-based guideline on the specific timing and nutrients to be adopted to decrease post-operative complication following congenital cardiac surgery.
This study has some limitations. Due to the scarcity of RCTs on this topic, we included non-experimental studies, however it was challenging that acceptance level is not normally distributed, and reliability cannot be collected without introducing bias, especially when using meta-analysis methods that rely on mean and standard deviation. Second, the early enteral nutrient was administered with different composition. Hence, there may be bias in the study outcomes.
The main strength of our study that all included studies were sound research design registered with clinical trials. All primary studies conducted from various parts of world and approved from institution’s review board or clinical registry. This review only included the infants undergoing congenital cardiac surgery therefore findings can replicable and provide highest evidence in hierarchy triangle
Authors recommended further RCTs with large sample sizes among infants undergoing congenital cardiac surgery. Additionally, all infants in the intervention groups received the same nutrition composition at the same time.
Conclusion
Enteral nutrition is a simple and often a substitute marker for post-operative recovery in routine clinical practice. However, there is a high prevalence of nutritional deficits among children, especially in post-operative patients. Nutrition therapy is an easy-to-administrator and can be administered based on postoperative records. EEN is a non-invasive, cost-effective, non-pharmacological intervention that can be implemented in clinical practice to improve patient well-being within adverse reactions. The efficacy of early nutrition has been published on cardiac disease in adults. However, some studies published on efficacy of early nutrition on gastrointestinal surgery in children. No systematic reviews have assessed the efficacy of EEN on post-operative outcome among infants undergoing congenital cardiac surgery. Therefore, it is an important to discuss which type of nutrition and time of first administration need to address. Therefore, it is crucial to discuss which type of nutrition and when the first administration should be addressed among infants after congenital heart surgery.
Acknowledgments
We are extremely thankful to Ms. Reetika Williams & Mrs.Sudha Janganure for editing English language and proof reading of our article.
Authors’ Contribution
Conceptualization: Kurvatteppa Halemani, Sanjay Dhiraaj, Latha Thimmappa, Alwin Issac.
Data curation: Kurvatteppa Halemani, Latha Thimmappa, Sanjay Dhiraaj.
Formal Analysis: Prabhaker Mishra, Sanjay Dhiraaj, Latha Thimmappa.
Methodology: Kurvatteppa Halemani, Sanjay Dhiraaj, Latha Thimmappa.
Project administration: Sanjay Dhiraaj.
Supervision: Prabhaker Mishra.
Validation: Sanjay Dhiraaj, Latha Thimmappa, Anu Mavinatop.
Visualization: Prabhaker Mishra, Latha Thimmappa.
Writing – original draft: Kurvatteppa Halemani, Sanjay Dhiraaj, Latha Thimmappa.
Writing – review & editing: Alwin Issac, Sanjay Dhiraaj.
COI-statement
The authors declare no conflict of interest in this study.
Ethical Approval
This project was a PROSPERO-registered systematic review and meta-analysis. Hence didn’t require ethical approval as no direct information or interventions were collected/performed on humans.
Funding
This systematic review and meta-analysis has not received financial support from any monetary resources.
Research Highlights
What is the current knowledge?
There are no clear guidelines, and systematic reviews have evaluated the impact of EEN on postoperative outcomes in infants undergoing congenital cardiac surgery.
What is new here?
This systematic review and meta-analysis yielded strong evidence that EEN reduced hospital stay and postoperative complications among infants undergoing post-operative cardiac surgery.
References
- World Health Organization (WHO). Birth Defects. Geneva: WHO; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/birth-defects. Accessed September 20, 2022.
- Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990-2017. Medicine (Baltimore) 2020; 99(23):e20593. doi: 10.1097/md.0000000000020593 [Crossref] [ Google Scholar]
- GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health 2020; 4(3):185-200. doi: 10.1016/s2352-4642(19)30402-x [Crossref] [ Google Scholar]
- Saxena A. Congenital heart disease in India: a status report. Indian Pediatr 2018; 55(12):1075-82. doi: 10.1007/s13312-018-1445-7 [Crossref] [ Google Scholar]
- Yun SW. Congenital heart disease in the newborn requiring early intervention. Korean J Pediatr 2011; 54(5):183-91. doi: 10.3345/kjp.2011.54.5.183 [Crossref] [ Google Scholar]
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002; 39(12):1890-900. doi: 10.1016/s0735-1097(02)01886-7 [Crossref] [ Google Scholar]
- Oster ME, Lee KA, Honein MA, Riehle-Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics 2013; 131(5):e1502-8. doi: 10.1542/peds.2012-3435 [Crossref] [ Google Scholar]
- Sables-Baus S, Kaufman J, Cook P, da Cruz EM. Oral feeding outcomes in neonates with congenital cardiac disease undergoing cardiac surgery. Cardiol Young 2012; 22(1):42-8. doi: 10.1017/s1047951111000850 [Crossref] [ Google Scholar]
- Owens JL, Musa N. Nutrition support after neonatal cardiac surgery. Nutr Clin Pract 2009; 24(2):242-9. doi: 10.1177/0884533609332086 [Crossref] [ Google Scholar]
- Ismail SR, Mehmood A, Rabiah N, Abu-sulaiman RM, Kabbani MS. Impact of the nutritional status of children with congenital heart diseases on the early post-operative outcome. Gaz Egypt Paediatr Assoc 2021; 69(1):28. doi: 10.1186/s43054-021-00077-9 [Crossref] [ Google Scholar]
- Huang HH, Hsu CW, Kang SP, Liu MY, Chang SJ. Association between illness severity and timing of initial enteral feeding in critically ill patients: a retrospective observational study. Nutr J 2012; 11:30. doi: 10.1186/1475-2891-11-30 [Crossref] [ Google Scholar]
- Fivez T, Kerklaan D, Mesotten D, Verbruggen S, Wouters PJ, Vanhorebeek I. Early versus late parenteral nutrition in critically ill children. N Engl J Med 2016; 374(12):1111-22. doi: 10.1056/NEJMoa1514762 [Crossref] [ Google Scholar]
- Green JPH. Cochrane Training. 2011. Available from: https://training.cochrane.org/handbook/PDF/v6.2. Accessed August 20, 2022.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4(1):1. doi: 10.1186/2046-4053-4-1 [Crossref] [ Google Scholar]
- Halemani K, Issac A, Mishra P, Mathias E. The impact of exercise on fatigue among patients undergoing adjuvant radiation therapy: a systematic review and meta-analysis. J Caring Sci 2022; 11(1):46-55. doi: 10.34172/jcs.2022.02 [Crossref] [ Google Scholar]
- Ehrmann DE, Harendt S, Church J, Stimmler A, Vichayavilas P, Batz S. Noncompliance to a postoperative algorithm using feeding readiness assessments prolonged length of stay at a pediatric heart institute. Pediatr Qual Saf 2017; 2(5):e042. doi: 10.1097/pq9.0000000000000042 [Crossref] [ Google Scholar]
- Yoshimura S, Miyazu M, Yoshizawa S, So M, Kusama N, Hirate H. Efficacy of an enteral feeding protocol for providing nutritional support after paediatric cardiac surgery. Anaesth Intensive Care 2015; 43(5):587-93. doi: 10.1177/0310057x1504300506 [Crossref] [ Google Scholar]
- Du N, Cui Y, Xie W, Yin C, Gong C, Chen X. Application effect of initiation of enteral nutrition at different time periods after surgery in neonates with complex congenital heart disease: a retrospective analysis. Medicine (Baltimore) 2021; 100(1):e24149. doi: 10.1097/md.0000000000024149 [Crossref] [ Google Scholar]
- Scheeffer VA, Ricachinevsky CP, Freitas AT, Salamon F, Rodrigues FFN, Brondani TG. Tolerability and effects of the use of energy-enriched infant formula after congenital heart surgery: a randomized controlled trial. JPEN J Parenter Enteral Nutr 2020; 44(2):348-54. doi: 10.1002/jpen.1530 [Crossref] [ Google Scholar]
- Sahu MK, Singal A, Menon R, Singh SP, Mohan A, Manral M. Early enteral nutrition therapy in congenital cardiac repair postoperatively: a randomized, controlled pilot study. Ann Card Anaesth 2016; 19(4):653-61. doi: 10.4103/0971-9784.191550 [Crossref] [ Google Scholar]
- Pillo-Blocka F, Adatia I, Sharieff W, McCrindle BW, Zlotkin S. Rapid advancement to more concentrated formula in infants after surgery for congenital heart disease reduces duration of hospital stay: a randomized clinical trial. J Pediatr 2004; 145(6):761-6. doi: 10.1016/j.jpeds.2004.07.043 [Crossref] [ Google Scholar]
- Chen X, Zhang M, Song Y, Luo Y, Wang L, Xu Z. Early high-energy feeding in infants following cardiac surgery: a randomized controlled trial. Transl Pediatr 2021; 10(10):2439-48. doi: 10.21037/tp-21-360 [Crossref] [ Google Scholar]
- Yu XR, Xie WP, Liu JF, Wang LW, Cao H, Chen Q. Effect of the addition of human milk fortifier to breast milk on the early recovery of infants after congenital cardiac surgery. Front Pediatr 2021; 9:661927. doi: 10.3389/fped.2021.661927 [Crossref] [ Google Scholar]
- Kalra R, Vohra R, Negi M, Joshi R, Aggarwal N, Aggarwal M. Feasibility of initiating early enteral nutrition after congenital heart surgery in neonates and infants. Clin Nutr ESPEN 2018; 25:100-2. doi: 10.1016/j.clnesp.2018.03.127 [Crossref] [ Google Scholar]
- Cui Y, Li L, Hu C, Shi H, Li J, Gupta RK. Effects and tolerance of protein and energy-enriched formula in infants following congenital heart surgery: a randomized controlled trial. JPEN J Parenter Enteral Nutr 2018; 42(1):196-204. doi: 10.1002/jpen.1031 [Crossref] [ Google Scholar]
- Liu JF, Xie WP, Lei YQ, Cao H, Yu XR, Chen Q. Effects of different feeding intervals on the feeding outcomes of infants who underwent surgical repair of ventricular septal defects. J Card Surg 2021; 36(11):4134-8. doi: 10.1111/jocs.15933 [Crossref] [ Google Scholar]
- Hill A, Nesterova E, Lomivorotov V, Efremov S, Goetzenich A, Benstoem C. Current evidence about nutrition support in cardiac surgery patients-what do we know? Nutrients 2018; 10(5):597. Current evidence about nutrition support in cardiac surgery patients-what do we know? Nutrients 2018; 10(5):597. doi: 10.3390/nu10050597 [Crossref] [ Google Scholar]
- Behera BK, Misra S, Tripathy BB. Systematic review and meta-analysis of safety and efficacy of early enteral nutrition as an isolated component of enhanced recovery after surgery [ERAS] in children after bowel anastomosis surgery. J Pediatr Surg 2022; 57(8):1473-9. doi: 10.1016/j.jpedsurg.2021.07.020 [Crossref] [ Google Scholar]
- Saxena A, Relan J, Agarwal R, Awasthy N, Azad S, Chakrabarty M. Saxena A, Relan J, Agarwal R, Awasthy N, Azad S, Chakrabarty M, et alIndian guidelines for indications and timing of intervention for common congenital heart diseases: revised and updated consensus statement of the Working Group on Management of Congenital Heart DiseasesAbridged Secondary Publication. Indian Pediatr 2020; 57(2):143-57. [ Google Scholar]
- Sousa-Uva M, Head SJ, Milojevic M, Collet JP, Landoni G, Castella M. 2017 EACTS guidelines on perioperative medication in adult cardiac surgery. Eur J Cardiothorac Surg 2018; 53(1):5-33. doi: 10.1093/ejcts/ezx314 [Crossref] [ Google Scholar]
- Giridhar VU. Role of nutrition in oral and maxillofacial surgery patients. Natl J Maxillofac Surg 2016; 7(1):3-9. doi: 10.4103/0975-5950.196146 [Crossref] [ Google Scholar]
- Flordelís Lasierra JL, Pérez-Vela JL, Umezawa Makikado LD, Torres Sánchez E, Colino Gómez L, Maroto Rodríguez B. Early enteral nutrition in patients with hemodynamic failure following cardiac surgery. JPEN J Parenter Enteral Nutr 2015; 39(2):154-62. doi: 10.1177/0148607113504219 [Crossref] [ Google Scholar]
- Preiser JC, Ichai C, Orban JC, Groeneveld AB. Metabolic response to the stress of critical illness. Br J Anaesth 2014; 113(6):945-54. doi: 10.1093/bja/aeu187 [Crossref] [ Google Scholar]
- Sullivan KJ, Chan E, Vincent J, Iqbal M, Wayne C, Nasr A. Feeding post-pyloromyotomy: a meta-analysis. Pediatrics 2016; 137(1). 10.1542/peds.2015-2550
- Greer D, Karunaratne YG, Karpelowsky J, Adams S. Early enteral feeding after pediatric abdominal surgery: a systematic review of the literature. J Pediatr Surg 2020; 55(7):1180-7. doi: 10.1016/j.jpedsurg.2019.08.055 [Crossref] [ Google Scholar]
- Halemani K, Shashidhara YN, D’Souza SRB. An evaluative study to assess the effectiveness of a video-assisted teaching module on knowledge and practice regarding home-based colostomy care of children among primary caregivers in selected hospital Lucknow, Uttar Pradesh. Indian J Surg Oncol 2021; 12(1):146-51. doi: 10.1007/s13193-020-01268-3 [Crossref] [ Google Scholar]
- Eskes AM, Schreuder AM, Vermeulen H, Nieveen van Dijkum EJM, Chaboyer W. Developing an evidence-based and theory informed intervention to involve families in patients care after surgery: a quality improvement project. Int J Nurs Sci 2019; 6(4):352-61. doi: 10.1016/j.ijnss.2019.09.006 [Crossref] [ Google Scholar]
- Larsen BM, Beggs MR. Nutrition support for the critically ill infant post cardiac surgery. In: Diet and Nutrition in Critical Care. New York, NY: Springer; 2016. p. 871-84. 10.1007/978-1-4614-7836-2_143
- Oyarzún I, Claveria C, Larios G, Le Roy C. Nutritional recovery after cardiac surgery in children with congenital heart disease. Rev Chil Pediatr 2018; 89(1):24-31. doi: 10.4067/s0370-41062018000100024 [Crossref] [ Google Scholar]