Journal of caring sciences. 13(1):12-19.
doi: 10.34172/jcs.2024.31919
Original Article
Development and Psychometric Evaluation of the Motivation for Healing Scale in Patients with Cancer
Fatemeh Hossieni Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Eesa Mohammadi Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, 2 
Reza Hosseini Data curation, Formal analysis, Project administration, Writing – original draft, 3 
Zohreh Sadat Investigation, Methodology, Supervision, Validation, Visualization, 4 
Negin Masoudi Alavi Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, 4, * 
Author information:
1Department of Community Health Nursing, School of Nursing and Midwifery, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
2Department of Nursing, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
3LinkedIn Corporation, Sunnyvale, CA, USA
4Trauma Nursing Research Center, Kashan University of Medical Sciences, Kashan, Iran
Abstract
Introduction:
This study was conducted to develop and validate a Motivation for Healing Scale (MHS) in Cancer.
Methods:
in this methodological study, the MHS draft was developed based on the approach of Waltz and colleagues using existing scales and concept analysis. The psychometric features, including face validity (qualitative and quantitative), content validity (qualitative and quantitative), structural validity (exploratory and confirmatory factors), and construct validity (convergent and discriminant validity) were assessed. Finally, the reliability was evaluated using internal consistency, and stability.
Results:
Based on the results of the qualitative phase, an initial item pool was generated with 55 items, Exploratory and confirmatory factor analyses were performed on the data collected from 404 patients. 25 Items were excluded during the psychometric evaluation phases. Reliability assessment and internal consistency assessment revealed that Cronbach’s alpha value of the 25-item MHS was 0.912. The results of intraclass correlation coefficient (0.93, 95% CI: 0.86– 0.96) showed the stability was strong.
Conclution:
The 25-item MHS is a valid and reliable scale for the assessment of motivation for healing in patients with cancer.
Keywords: Factor analysis, Healing, Motivation, Psychometric, Cancer
Copyright and License Information
© 2024 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
This is an approved PhD. thesis by the Vice Chancellor for Research (VCR) at Kashan University of Medical Science.
Introduction
Motivation refers to processes that stimulate and sustain goal-directed activities. Motivation leads to outcomes such as choice, effort, achievement, persistence, and environmental regulation.1 Motivation is an important concept in psychology and bearing complications and participating in rehabilitation and treatment programs.2 Lack of motivation can often result in patients dropping out of treatment, failing to comply with the prescribed treatment, experiencing relapse, and ultimately leading to negative outcomes.3
Motivation definition varies according to the type of disease and situation.2 Nowadays, cancer treatments are generally provided on an outpatient basis and patients need to be actively involved in treatment programs.2,4 The longer duration of treatments in cancer patients is likely associated with poor adherence to treatment, and treatment discontinuation.2,5
Poor medication adherence is a global issue, especially among patients with chronic diseases. In developed countries, only 50% of these patients adhere to their prescribed medications.6 Patients with cancer are generally expected to be highly motivated due to the importance of their disease, this does not always appear. Their treatment is associated with poor compliance and adherence rates.5 While some patients might have a strong motivation for healing, “healing is the personal experience of transcending suffering and transforming to wholeness”7 others might require support, and encouragement. These are a cause of concern for clinicians, patients and health care systems alike, since noncompliance is associated with poorer outcomes and higher health care costs.5,8
Nurses have a crucial role in enhancing patients’ motivation by utilizing various techniques. For this purpose, nurses need to measure the cancer patients’ motivation with a reliable and valid scale.9 Motivation assessment can increase our understanding of whether individual copes with a cancer diagnosis and what might be his/her behaviors during the treatment process.10
Despite the importance of motivation for cancer healing, we did not find any questionnaire for measuring this variable. The questionnaires used in previous research are not specific to cancer patients, and the concept of motivation in cancer patients has not been clearly defined in these questionnaires.9
The aim of the study was to develop a valid and reliable scale in order to determine the motivation of healing in cancer patients.
Materials and Methods
This methodological study was conducted from November 2019 to June 2022 in the following phases. Production phases of the Motivation for Healing Scale (MHS) in cancer are presented in Figure 1.
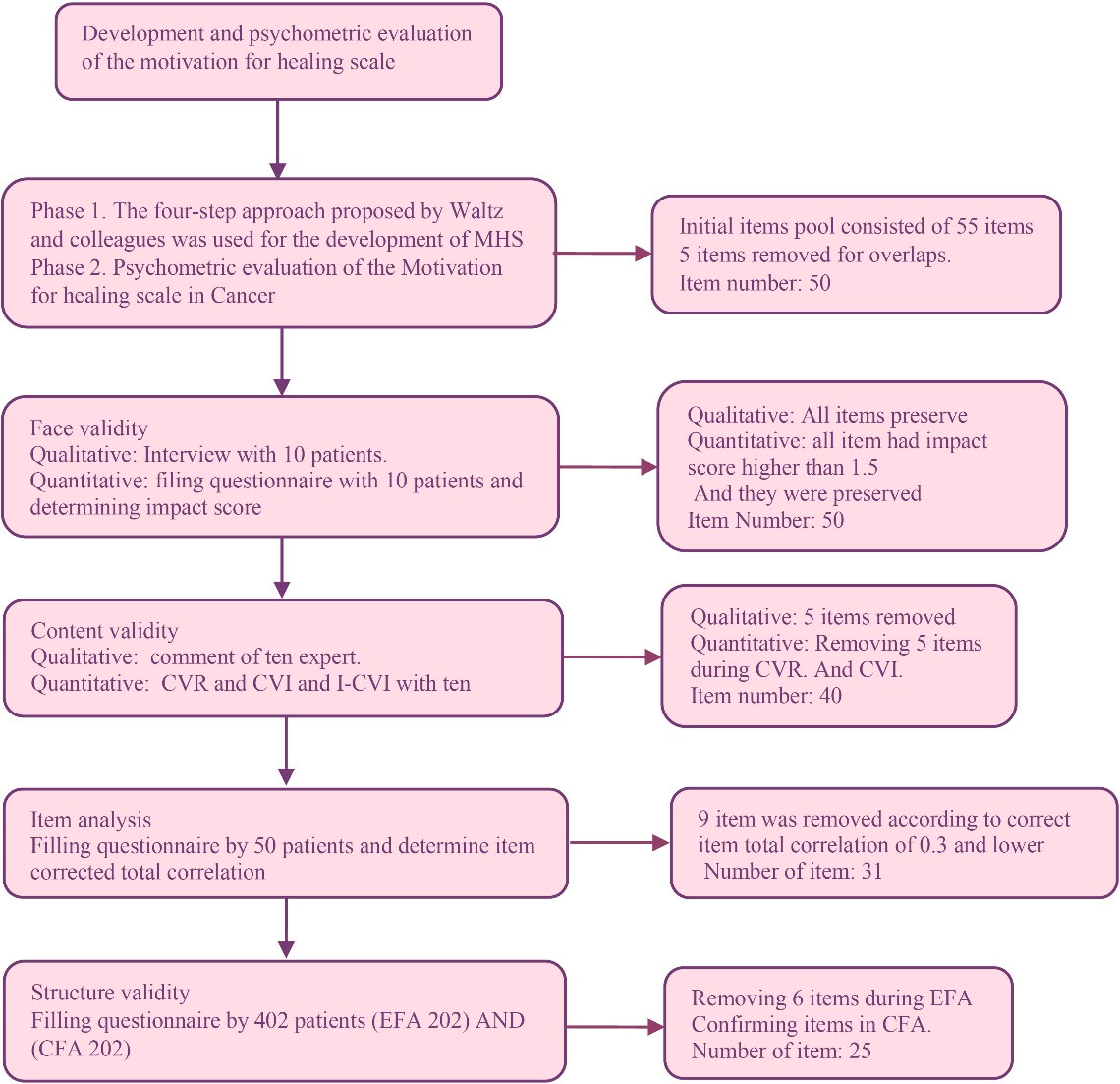
Figure 1.
Production phases of the motivation for healing scale in cancer
.
Production phases of the motivation for healing scale in cancer
Phase I: The four-step approach proposed by Waltz and colleagues was used for the development of MHS.
Step I: a qualitative research approach was used to define motivation for healing in cancer patients.11 Data were collected through individual semi-structured interviews and the themes were derived from the data using the content analysis method. This method generally describes a phenomenon when limited research/theories are available in that field. This method was selected to obtain new and rich data sets.12 The participants consisted of 34 cancer patients. Qualitative phase of this study was published elsewhere with title motivation for healing in cancer patients.13
Step II: measurement goals were defined based on the identified definitions in the qualitative steps.
Step III: the more specific domains of the questionnaire and the number of their items were determined.
Step IV: items were generated and literature reviews were conducted in the item generation phase. The literature reviews phase of this study was published.9 The scoring method was set as the five-point Likert scale from completely agree to disagree.11
Phase II: Psychometric properties of MHS were assessed in the following three steps:
Step I: Face validity was assessed through quantitative and qualitative methods. Quantitative face validity was calculated by determining the item impact score for each item of the scale with acceptable level of≥1.5.11 Ten cancer patients were asked to score the importance of each item. Next, qualitative face validity of the scale was evaluated by 10 patients. Cancer patients read items and released their comments on the simplicity and clarity of them.
The content validity of the questionnaire was evaluated by both qualitative and quantitative methods.14 Ten experts with expertise and experience in psychometric assessment (n=4), psychology (n=2), oncologist (n=2), and nursing (n=2) were requested to apply their analysis of the scale in terms of grammar, phrasing, item allocation, and scaling to assess the qualitative content validity. Their recommendations were considered in the scale.15 The quantitative content validity was examined by calculating the content validity ratio (CVR) and content validity index (CVI). The same 10 experts then specified each item’s necessity for the CVR evaluation. Based on the Lawshe formula, when 10 experts’ opinions are considered, The CVR is calculated as more than 0.62 is acceptable.
CVI was calculated; experts rated the relevancy of the items on 4-point Likert type scale (not relevant, requiring overall revision, relevant but requiring brief revision, completely irrelevant).16 In addition, the mean of CVI scores is taken into account to measure the scale content (I-CVI average for all items on the scale). A score of 0.8 is considered appropriate.17 But, for items, if there was an item with I-CVI less than 0.78, it was removed.18 Based on the above considerations, 10 items were removed in this step, and the items of MHS were reduced to 40 items.
Step II: Items selection process: After evaluation of the content validity of the scale, item analysis was performed to examine the internal consistency of the scale and to find inappropriate items. The scale was given to 50 patients to complete. Their responses were used to assess the internal consistency of the scale. The items with an inter-item correlation value of less than 0.3 were removed. Moreover, items with a high correlation (r ≥ 0.70), should be merged into one item.
This exploratory factor analysis (EFA) was evaluated through principal axis factoring and oblimin rotation. Bartlett’s test and the Kaiser-Meyer-Olkin (KMO) index were used to determine the suitability of data for factor analysis. The number of factors was determined based on scree plot and an eigenvalue of more than 119(Figure 2). A confirmatory factor analysis (CFA) was conducted to assess the structural factors (Figure 3). The fitness indices of the scale include comparative fit index (CFI), goodness-of-fit-index (GFI), adjusted goodness-of-fit index (AGFI), normed fit index (NFI), and root mean square error of approximation (RMSEA). In this step, factors with factor loading less than 0.5 were removed from the model.
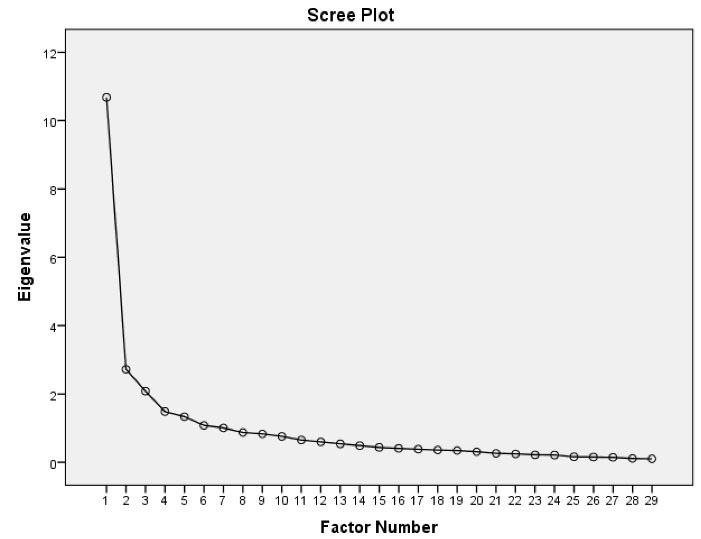
Figure 2.
The scree plot of the factor structure of MHS in factor analysis
.
The scree plot of the factor structure of MHS in factor analysis
Multivariate Normality and Outliers
Multivariate outliers were assessed using the Mahalanobis d-squared test (P<0.001). Univariate normality was checked using skewness (±3) and kurtosis (±8).
Step III: The internal consistency of MHS and its subscales were evaluated using Cronbach’s alpha calculation. Additionally, the stability of the measurement was assessed by randomly selecting 30 patients from the study sample and asking them to re-answer MHS. The correlation between the test and retest scores was then determined by calculating the intraclass correlation coefficient (ICC). Furthermore, the standard error measurement of agreement and the smallest detectable change (SDC) were calculated.20
Data gathering: In the current study, the sample size for EFA is between 5 and 10 for each item.18 202 samples for EFA and another 202 samples to evaluate the CFA. Inclusion criteria were: being diagnosed with cancer; being 18 and older; being aware of their disease; being under treatment, and patients were excluded if they had a previous history of psychiatric illness and/or on regular treatment with the psychotropic (We asked them before the study). Participants were selected via quota sampling from two hospitals and chemotherapy wards. The first author collected the data using self-reported questionnaires.
Scale: The data collected consisted of a demographic questionnaire and the primary version of MHS. The demographic questionnaire included age, gender, marital status, educational level, method of treatment, type of cancer, and duration of the disease. The primary version of MHS after the qualitative phase contained 50 items in seven domains: Fear and alertness to preserve life (10 items), willingness to live (17 items), trust in the treatments (4 items), positive thinking ability (6 items), trust in superior powers (4-items), sense of belongingness (4-items), and sense of responsibility (5-items). Items were scored on a five-point Likert scale.
Data analysis was performed via SPSS software (v. 16.0) in conjunction with “psych” and “lavaan” packages in R (https://www.r-project.org/).
Results
In this study, the basis for preparing the item pool was content analysis and the literature review. Based on the results of the interviews, three main themes and seven categories were determined. The themes were identified as (I) desire to survive; (II) spirit of optimism; (III) belongingness and responsibility. The qualitative phase of this study was published. For more detailed information please refer to it.13
The first researcher, with the help of other research team members, extracted the appropriate items based on operation definitions of the themes extracted from the content analysis. The goal was to have a relatively comprehensive set of possible items, and to that end, no initial limit was set to the number of items.
The initial pool of 55 items was examined (for overlaps) in several sessions and 50 items were approved for the psychometric phase. In the qualitative content validity assessment, the wording of some items was also changed and five items were excluded due to their overlaps with other items. Production phases of the motivation for healing scale in cancer show in Figure 1.
In the second phase, in the qualitative face validity of the scale, all items have acceptable impact scores. After the qualitative face validity, six items of the scale were revised according to the patients’ idea.
The quantitative content validity assessment, CVR, and CVI of the items were calculated and the items with CVI less than 0.78, or CVR less than 0.62 were removed from the questionnaire. Five items were removed because of low CVI, or CVR.
The scale was given to 50 patients similar to the main study sample and asked them to complete the MHS and Cronbach’s alpha value was estimated to be 0.93. In addition, 9 items with inter-item correlation coefficients smaller than 0.3 were excluded and 31 items remained on the scale for further psychometric evaluation.
For construct validity assessment, EFA was conducted. 202 patients were recruited to fill out 31-item MHS. Most of them were female (54%) and married (81%). The mean (SD) of their age was 52.50 (13.84) years old. Other characters can be seen in Table 1.
Table 1.
The demographic characteristics of the participants
|
Variable
|
No. (%)
|
| Gender |
|
| Male |
204 (50) |
| Female |
200 (49) |
| Marital status |
|
| Married |
324 (80) |
| Single |
80 (20) |
| Type of the cancer |
|
| Skin |
14 (3.3) |
| Lung |
34 (8.2) |
| Bone |
38 (9.1) |
| Gastrointestinal (GI) |
94 (22.5) |
| Breast |
102 (24.5) |
| Bladder cancer |
26 (6.2) |
| Liver |
20 (4.9) |
| Ovarian |
18 (4.3) |
| Other cancers |
62 (17) |
| Educational level |
|
| Illiterate |
72 (18.3) |
| Primary |
154 (37) |
| Diploma |
98 (26) |
| Above Diploma |
78 (18.7) |
| Type of treatment |
|
| Chemotherapy |
198 (48) |
| Radiotherapy |
114 (28) |
| Chemotherapy and radiotherapy |
78 (19.2) |
| Other treatments |
18 (4.8) |
The KMO test indicated KMO adequacy (test value = 0.90), and Bartlett’s test revealed that the matrix of inter correlations among items was appropriate for factor analysis (P<0.001). In the next step, the number of commonalities was examined, which was less than 0.02 in items 12 and 21 showing that these items had little in common with other items. Therefore these items were removed from the EFA. Other items had several commonalities of more than 0.2.
In the EFA, initially, the number of factors was determined to be 6 using Eigen-values larger than 1. In the next step, the items were analyzed by the method ofprincipal axis factoring and oblimin rotation. Finally, 5 factors were found to be appropriate by (a) requiring each factor to correspond to at least 3 items; (b) each item is highly correlated ( > 0.4) with one and only one factor (no crossover) resulting in the elimination of 4 items. (c) Each factor explains at least 5% of the total variance. The parallel analysis scree plots of structure also confirmed 5 factors for MHS. Scree plot was used to predict the number of factors (Figure 2).
The remaining 25 items in the questionnaire that were loaded on five factors showed an absolute consistency with categories in the qualitative phase. These factors could explain 51.32% of the total variance of the MHS score. Items and their loadings can be seen in Table 2. The minimum and maximum possible total scores of MHS were 25 and 125. A higher score indicates higher motivation for healing. The floor and ceiling effects of the scale were 0% and 10% respectively (range 0–0.10). The time required to answer the scale was 15 minutes (including demographic questions).
Table 2.
The items of the extracted factors and their factor loading values
|
Items
|
Factor loading
|
h2
|
λ
|
Variance
|
Ω
|
Α
|
| Sense of belongings and responsibility |
|
|
|
|
|
|
| Q35 Love of family has made me strive for healing |
0.85 |
0.88 |
2.89 |
11.6 |
0.90 |
0.85 |
| Q36 This thought that I can be more with my beloved ones gives me energy |
0.79 |
0.78 |
| Q37 There are people in my life who lovingly support and care for me |
0.67 |
0.51 |
| Q39 I strive for healing because my family needs my care and support for continuing life |
0.51 |
0.34 |
| Q40 I strive for healing because then, I can help my family to have a better future |
0.63 |
0.64 |
| Trust in superior Powers |
|
|
|
|
|
|
| Q22 Believing in God’s will make me hopeful for overcoming the disease |
0.67 |
0.65 |
2.53 |
10.01 |
0.83 |
0.85 |
| Q23 I consider the disease as a Divine trial, which I need to try to achieve success in it |
0.88 |
0.74 |
| Q24. I believe that God will give me the ability to overcome the disease |
0.59 |
0.50 |
| Q25. Believing in miracles and Divine healing makes me hopeful about recovery |
0.79 |
0.63 |
| Willingness to live |
|
|
|
|
|
|
| Q7. I want to achieve healing to fulfill my incomplete responsibilities in life |
0.51 |
0.40 |
2.69 |
10.76 |
0.86 |
0.84 |
| Q8. I want to achieve healing to fulfill my wishes and plans for my future |
0.62 |
0.46 |
| Q9. determined to regain my physical health due to my interest in my pre-illness life |
0.73 |
0.64 |
| Q10. I want to achieve healing to enjoy my possessions such as my job, education, and financial facilities |
0.81 |
0.66 |
| Q11 Healing is important to me to be able to participate in rituals (such as religious ceremonies, weddings, and parties) and group activities (such as sports) |
0.56 |
0.36 |
| Q13 I want to achieve healing to enjoy life and its beauties |
0.53 |
0.46 |
| Positive thinking ability |
|
|
|
|
|
|
| q18. I feel I have the ability to continue the treatment |
0.51 |
0.29 |
2.41 |
9.68 |
0.75 |
0.78 |
| q20. I’m determined to fight the disease and surrender to it |
0.47 |
0.34 |
| q26. I believe that the course of the disease and treatment is transient and will eventually finish |
0.56 |
0.45 |
| q27. I give hope to myself for healing and try to maintain my morale |
>0.67 |
0.51 |
| q28. I feel lucky though I’m ill and this feeling makes me hopeful about treatment’s future |
0.61 |
0.39 |
| q29. Familiarity with healed patients boosts my hope |
0.60 |
0.42 |
| Trust in the treatment |
|
|
|
|
|
|
| q30. Believing in a physician’s proficiency in treatment has made me hopeful |
0.73 |
0.65 |
2.33 |
9.35 |
0.85 |
0.85 |
| q31. Believing in the proficiency of the nurses’ who care for me has made me hopeful |
0.73 |
0.74 |
| q32. I’m hopeful about scientific advancements and the discovery of new treatments for my disease |
0.70 |
0.50 |
| q33. Believing in the effectiveness of medications has made me hopeful about my treatment |
0.63 |
0.63 |
Note: the minimum factor load is 0.4; factors<0.4 are not listed in the table. Abbreviation: ʎ Eigenvalue, h2 commonality.
A CFA was conducted to assess the structural factors. The model fitness was assessed by six indices: The fitness indices of the scale include CFI 5.90, GFI 0.86, AGFI 0.90, NFI 0.84, and RMSEA 0.04 (Figure 3). Shows the path diagram after the CFA.
Reliability assessment and internal consistency assessment revealed that Cronbach’s alpha value of the 25-item MHS was 0.912. Finally, the stability of scale was strong based on the overall ICC result (0.93, 95% CI: 0.86 –0.96). The standard error of measurement and SDC (with a 95% confidence interval) were 2.7 and 7. 5, respectively (Table 3). Findings revealed that the 25-item MHS had acceptable validity and reliability in cancer patients and could determine the score of motivation in the range of 25-125.
Table 3.
The reliability measurements of MHS (Number of items, % of Variance, α, SEM, SDC )
|
Factors
|
Items
|
α
|
ICC (95% CI)
|
SD
|
SEM
|
SDC
|
| Sense of belongings and responsibility |
5 |
0.93 |
0.91 (0.82-0.94) |
1.4 |
0.4 |
1.10 |
| Trust in superior powers |
4 |
0.90 |
0.91 (0.83 -0.93) |
2.7 |
0.75 |
2.07 |
| Willingness to live |
6 |
0.76 |
0.78 (0.58-0.89) |
2.9 |
1.36 |
3.76 |
| Positive thinking ability |
4 |
0.86 |
0.87 (0.73-0.94) |
2.3 |
0.88 |
2.4 |
| Trust in the treatment |
6 |
0.88 |
0.86 (0.93 -0.72) |
2.2 |
0.98 |
2.7 |
| Total Items of MHS |
25 |
0.93 |
0.92 (0.96 -0.86) |
10.2 |
2.7 |
7.5 |
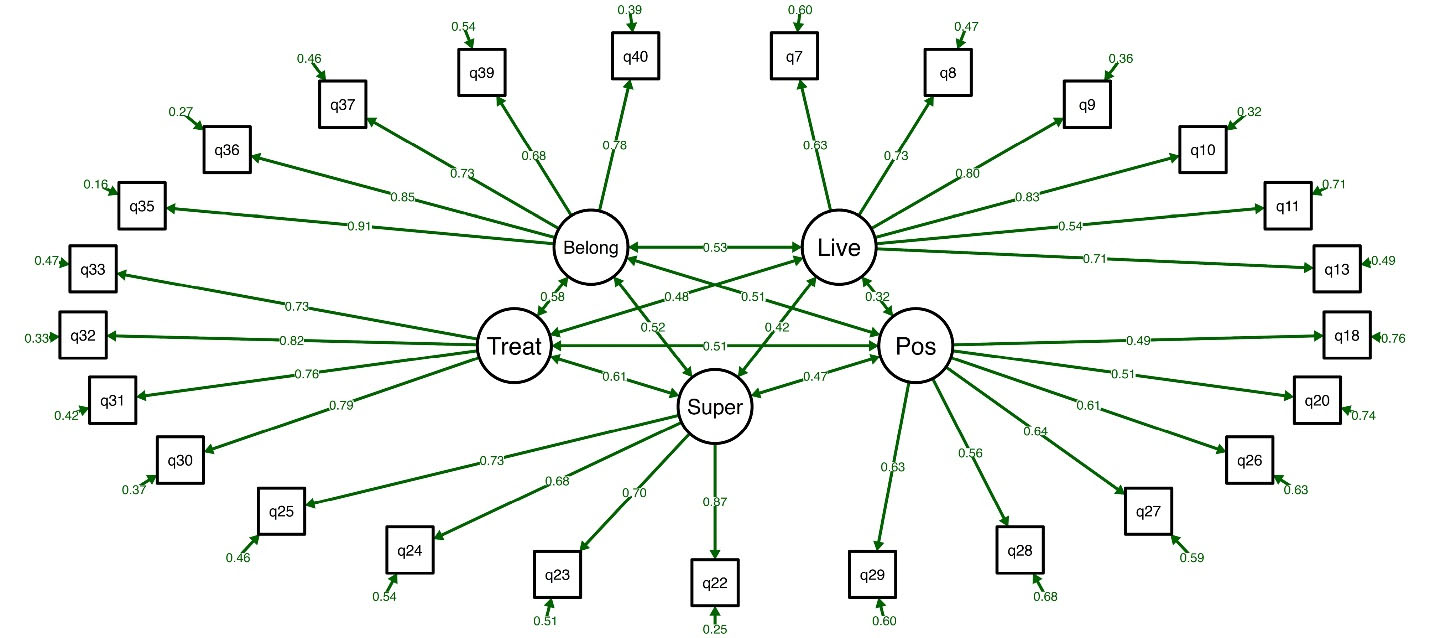
Figure 3.
Model of first-order confirmation factor analysis. Abbreviations: Belong, Sense of belongings and responsibility;Super: Trust in superior; Live, live willingness to live; Treat, Trust in thetreatment; Pos, Positive thinking ability
.
Model of first-order confirmation factor analysis. Abbreviations: Belong, Sense of belongings and responsibility;Super: Trust in superior; Live, live willingness to live; Treat, Trust in thetreatment; Pos, Positive thinking ability
Discussion
Based on the results of this study, the MHS is the valid and reliable scale to assess the motivation for healing in cancer patients. It contains 25 items that were divided into five factors. “Sense of belongings and responsibility” with five items “Trust in superior powers” with four items “Willingness to live” with 6 items “positive thinking ability” with four items.
Motivation plays an important role in the healing of people. It is important to have a means of assessing motivation for healing. Scales exist to measure motivation in normal and medically ill populations but not in people with cancer. Thus, we developed a self-report scale to measure motivation for healing in cancer. The scale started with the 55 original items used to assess motivation for healing in cancer, based on the motivational concepts of the qualitative phase and literature review.
Initial item selection, internal consistency, and test reliability analyses from a convenience cancer subsample and a comparative group of normal reduced the scale to 50 items for psychometric validation in the cancer sample. In EFA, five factors were extracted. In this study, factors and validity analyses for the cancer sample resulted in a final recommended set of 25-items.
The scales that have been designed to measure patients’ motivation in clinical settings were 34 scales presented in scoping review9; 6 of 34 scales were newly developed to measure patients’ motivation. Four of six scales were developed or tested with patients who had a mental illness diagnosis.21-24 One scale was developed for patients with substance abuse disorder25 and another scale was developed for patients who have a brain injury.22
The most important step to designing reliable and valid measurement scales for the assessment of patients’ motivation is considering the patient’s experiences. This study used a qualitative approach (content analysis) to define motivation for healing and its dimensions in cancer settings according to the patient’s experiences. Thus, a more accurate criterion can be achieved for assessing a patient’s motivation.
Face validity assessment in the present study also showed the acceptable face validity of MHS. Face validity refers to the comprehensibility of the items for the target population.11the acceptable face validity of MHS denotes that its items are comprehensible for cancer patients. Other scales reported some form of validity evidence but missing several criteria regarding their assessment of content validity during initial measure development, and experts or members of the target population were not consulted. The result was that items were often not matched to the dimensions of the construct.9 Content validity assessment based on the comments of experts in different specialties revealed a scale-level CVI of 0.97. Scale-level CVI values greater than 0.90 are acceptable and represent an essential component of scale development18 because it shows that experts believe the items of the intended scale accurately measure the intended concept.
EFA in this study revealed that MHS consists of five subscales. These subscales accounted for 51.2% of the total variance of the motivation for healing score. A scale is considered to have acceptable construct validity when its subscales explain at least 50% of its total variance.26 In the development of other scales, researchers used factor analysis in varying ways.22,25,27 principal components analysis (PCA) with varimax rotation was used in one scale,21 and one of the scales used EFA with oblimin rotation.23 Unfortunately, most articles that introduced these scales did not explain how to choose the type of factor analysis.
Our findings revealed that MHS does not have ceiling and floor effects. These effects are present when more than 15% of respondents obtain respectively the maximum and the minimum possible total scores of the intended scale.
The presence of these effects indicates low content validity. The Cronbach’s α coefficient of MHS was 0.912. Cronbach’s α coefficients greater than 0.70 are acceptable. Thus, MHS has acceptable internal consistency and reliability.19 Internal consistency was considered in all 6 patient motivation scales21-25,27; and Cronbach’s α coefficient’s estimate for all the scales and subscales ranged from 0.75 to 0.98.
Moreover, the test-retest ICC of MHS was 0.912 (P < 0.001). ICC values greater than 0.7 are acceptable and show the stability of the intended scale. Stability or repeatability assessment is among the methods for reliability assessment.19Therefore, the study showed the acceptable reliability of MHS. The SEM of MHS was 2.5 and its SDC was 7.2. Small SEM supports scale stability. A SEM of 2.5 in the possible range of 25-125 for the total score of MHS is considered very small and denotes the stability, repeatability, and reliability of the MHS. Information about measurement errors, such as the availability of two measurements or a calculation of measurement error, was recorded by two reviewed scales.23,24 So MHS could be used for a successful motivation for healing in cancer patient assessment.
Conclusion
The 25-item MHS has acceptable validity and reliability. Future studies in the area of patient motivation for healing are recommended with the use of MHS in research and care.
To our knowledge, this is the first scale that can measure the motivation for healing in cancer patients that has been developed in an exploratory mixed-method study, using both qualitative and quantitative methods. The developed scale needs to be used in different studies in different cultures and settings to show its usefulness over time. Interpretability explores the distribution of scores among groups and therefore was beyond the aim of this study. The scale has been developed in the Persian language then it has been translated into English. The validity and reliability of the English version of the scale need further investigation.
Acknowledgements
We sincerely acknowledge the authorities of Kashan University of Medical Sciences, nurses, patients and their families who helped to conduct this study.
COI-statement
The authors have no competing interests to declare that are relevant to the content of this article.
Data Availability Statement
The datasets are available from the corresponding author on reasonable request.
Ethical Approval
This study was approved by the Ethical Committee of Kashan University of Medical Sciences with the ethics code of KAUMS.NUHEMP.REC.1398.053. Informed consent from all participants has received additional legally authorized representatives of illiterate participants provided. All methods of study were performed by the relevant guidelines and regulations.
Research Highlights
What is the current knowledge?
What is new here?
References
- Schunk DH, DiBenedetto MK. Motivation and social cognitive theory. Contemp Educ Psychol 2020; 60:101832. doi: 10.1016/j.cedpsych.2019.101832 [Crossref] [ Google Scholar]
- Shankar S, Miller WC, Roberson ND, Hubley AM. Assessing patient motivation for treatment: a systematic review of available tools, their measurement properties, and conceptual definition. J Nurs Meas 2019; 27(2):177-209. doi: 10.1891/1061-3749.27.2.177 [Crossref] [ Google Scholar]
- Alfonsson S, Olsson E, Hursti T. Motivation and treatment credibility predicts dropout, treatment adherence, and clinical outcomes in an internet-based cognitive behavioral relaxation program: a randomized controlled trial. J Med Internet Res 2016; 18(3):e52. doi: 10.2196/jmir.5352 [Crossref] [ Google Scholar]
- Greer JA, Jackson VA, Meier DE, Temel JS. Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin 2013; 63(5):349-63. doi: 10.3322/caac.21192 [Crossref] [ Google Scholar]
- Hadji P, Blettner M, Harbeck N, Jackisch C, Lück HJ, Windemuth-Kieselbach C. The Patient’s Anastrozole Compliance to Therapy (PACT) Program: a randomized, in-practice study on the impact of a standardized information program on persistence and compliance to adjuvant endocrine therapy in postmenopausal women with early breast cancer. Ann Oncol 2013; 24(6):1505-12. doi: 10.1093/annonc/mds653 [Crossref] [ Google Scholar]
- Chauke GD, Nakwafila O, Chibi B, Sartorius B, Mashamba-Thompson T. Factors influencing poor medication adherence amongst patients with chronic disease in low-and-middle-income countries: a systematic scoping review. Heliyon 2022; 8(6):e09716. doi: 10.1016/j.heliyon.2022.e09716 [Crossref] [ Google Scholar]
- McElligott D. Healing: the journey from concept to nursing practice. J Holist Nurs 2010; 28(4):251-9. doi: 10.1177/0898010110376321 [Crossref] [ Google Scholar]
- Hadji P. Menopausal symptoms and adjuvant therapy-associated adverse events. Endocr Relat Cancer 2008; 15(1):73-90. doi: 10.1677/erc-07-0193 [Crossref] [ Google Scholar]
- Hosseini F, Masoud Alavi N, Mohammadi E, Sadat Z. Scoping review on the concept of patient motivation and practical tools to assess it. Iran J Nurs Midwifery Res 2021; 26(1):1-10. doi: 10.4103/ijnmr.IJNMR_15_20 [Crossref] [ Google Scholar]
- Argyriadi A, Argyriadis A. Psychological issues related to patients with cancer: the role of psychological, cultural, social and medical factors. Imp J Interdiscip Res 2019; 5(5):88-98. [ Google Scholar]
- Waltz CF, Strickland OL, Lenz ER. Measurement in Nursing and Health Research. New York: Springer Publishing Company; 2010. Available from: https://dl.uswr.ac.ir/bitstream/Hannan/138859/1/9780826105080.pdf. Accessed September 20, 2023.
- Kyngäs H. Inductive content analysis. In: Kyngäs H, Mikkonen K, Kääriäinen M, eds. The Application of Content Analysis in Nursing Science Research. Cham: Springer; 2020. p. 13-21. 10.1007/978-3-030-30199-6_2
- Hosseini F, Masoud Alavi N, Mohammadi E, Sadat Z. Motivation for healing in cancer patients: a qualitative study. Iran J Nurs Midwifery Res 2021; 26(6):555-61. doi: 10.4103/ijnmr.IJNMR_232_20 [Crossref] [ Google Scholar]
- Polit D, Beck C. Essentials of Nursing Research: Appraising Evidence for Nursing Practice. 10th ed. Philadelphia: Lippincott Williams & Wilkins; 2021.
- Ayre C, Scally AJ. Critical values for Lawshe’s content validity ratio: revisiting the original methods of calculation. Meas Eval Couns Dev 2014; 47(1):79-86. doi: 10.1177/0748175613513808 [Crossref] [ Google Scholar]
- Curtis AC, Keeler C. Measurement in nursing research. Am J Nurs 2021; 121(6):56-60. doi: 10.1097/01.NAJ.0000753668.78872.0f [Crossref] [ Google Scholar]
- Aning KS, Suranata K, Dwiarwati KA. Pengembangan instrumen pengukuran prokrastinasi siswa sekolah menengah pertama. SCHOULID Indones J School Counseling 2021; 6(3):174-82. doi: 10.23916/0086223293-00-0 [Crossref] [ Google Scholar]
- Polit D, Beck C. Resource Manual for Nursing Research: Generating and Assessing Evidence for Nursing Practice. 11th ed. Lippincott Williams & Wilkins; 2020.
- Hair JF Jr, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis. 7th ed. New York: Prentice Hall; 2010.
- Mardia KV. Measures of multivariate skewness and kurtosis with applications. Biometrika 1970; 57(3):519-30. doi: 10.1093/biomet/57.3.519 [Crossref] [ Google Scholar]
- Pelletier LG, Tuson KM, Haddad NK. Client motivation for therapy scale: a measure of intrinsic motivation, extrinsic motivation, and amotivation for therapy. J Pers Assess 1997; 68(2):414-35. doi: 10.1207/s15327752jpa6802_11 [Crossref] [ Google Scholar]
- van Beek N, Verheul R. Motivation for treatment in patients with personality disorders. J Pers Disord 2008; 22(1):89-100. doi: 10.1521/pedi.2008.22.1.89 [Crossref] [ Google Scholar]
- Jochems EC, Mulder CL, Duivenvoorden HJ, van der Feltz-Cornelis CM, van Dam A. Measures of motivation for psychiatric treatment based on self-determination theory: psychometric properties in Dutch psychiatric outpatients. Assessment 2014; 21(4):494-510. doi: 10.1177/1073191113517928 [Crossref] [ Google Scholar]
- Drieschner KH, Boomsma A. The treatment motivation scales for forensic outpatient treatment (TMS-F): construction and psychometric evaluation. Assessment 2008; 15(2):224-41. doi: 10.1177/1073191107311650 [Crossref] [ Google Scholar]
- Ryan RM, Plant RW, O’Malley S. Initial motivations for alcohol treatment: relations with patient characteristics, treatment involvement, and dropout. Addict Behav 1995; 20(3):279-97. doi: 10.1016/0306-4603(94)00072-7 [Crossref] [ Google Scholar]
- Reio TG Jr, Shuck B. Exploratory factor analysis: implications for theory, research, and practice. Adv Dev Hum Resour 2015; 17(1):12-25. doi: 10.1177/1523422314559804 [Crossref] [ Google Scholar]
- Chervinsky AB, Ommaya AK, deJonge M, Spector J, Schwab K, Salazar AM. Motivation for traumatic brain injury rehabilitation questionnaire (MOT-Q): reliability, factor analysis, and relationship to MMPI-2 variables. Arch Clin Neuropsychol 1998; 13(5):433-46. doi: 10.1093/arclin/13.5.433 [Crossref] [ Google Scholar]