Journal of caring sciences. 13(1):44-53.
doi: 10.34172/jcs.2024.31955
Original Article
Barriers and Facilitators during Community Reintegration of People with Spinal Cord Injury: A Qualitative Study
Meenakshi Mohan Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, * 
Roumi Deb Project administration, Supervision, Validation, Visualization, Writing – review & editing, 
Author information:
1Center for Anthropology, Department of Anthropology, AISS, Amity University, Uttar Pradesh Sector-125, Noida
Abstract
Introduction:
Spinal cord injury (SCI) individuals face challenges in community reintegration due to various factors. This study explores the barriers and facilitators affecting their reintegration, aiming to understand and address their diverse needs and challenges in different cultural contexts.
Methods:
The present qualitative study was conducted between December 2021 to June 2022 among 71 SCI individuals as data saturation was achieved. Data was collected via structured in-depth interview. Participants were identified through purposive sampling method, admitted, or visited to rehabilitation center, India. Data was analyzed according to Braun and Clarke’s thematic analysis method using MAXQDA 2020.
Results:
Data analysis led to the emergence of four major themes and several sub-themes specific to the single problem domain. The four major themes of barriers included environmental, cultural, psychological and health-related barriers. However, four facilitators (Family support, financial stability, religious practices, friends and leisure activity) came up which may help in overcoming from the challenges faced by the SCI individuals.
Conclusion:
People with SCI face various problems in their care, management and social lives. It is important to give attention to their needs along with comprehensive health support and strengthen the patient-provider interaction. This may generate a sense of self efficacy, self-esteem and promotes the mental well-being of people with spinal cord injuries. Working on the above mentioned issues can help SCI people in low- and middle-income countries become more integrated into their communities.
Keywords: Low-middle income countries, Spinal cord injuries, Challenges, Facilitators, Qualitative study
Copyright and License Information
© 2024 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
This research did not receive any type of grant from funding agencies in the public, private, commercial, or not-for-profit sectors.
Introduction
The International Classification of Functioning, Disability and Health (ICF) defines participation as incorporating the concept of “involvement,” which can mean taking part, being included or engaged in an area of life, being accepted, or having access to required resources and being an lively and contributing member of family as well as in social groups/society as a whole.1 Researchers discussed about the multifaceted nature of participation after the onset of spinal cord injury (SCI), its consequences and factors which influence the sufferers’ participation back into the community with various methods and approaches. Unfortunately, the progress of improving the long-term health and community inclusion are not uniform across the globe.2,3 Delays are very common between the initial injury and reaching to the specialized center for further treatment especially in resource poor countries.4 Secondary complications majorly pressure sores are the primary reason of morbidity and mortality. Furthermore, lack of appropriate and feasible medical equipment/s i.e. improper and uncomfortable wheelchairs, absence of healthcare facilities, societal attitudes, architectural characteristics, transportation as well as poor follow-up rates are the foremost elements for poor reintegration into the community.5,6
Very few research studies that have undertaken an in-depth examination of the challenges faced by individuals with SCIs in terms of their integration into the community and the identification of factors that assist them in surmounting these barriers. This knowledge gap becomes particularly noticeable in the unique context of a developing nation like India, characterized by substantial disparities in cultural norms, geographical conditions, available resources, opportunities, and the healthcare system when compared to the Western world. Nevertheless, it is of utmost importance to meticulously document these hindrances and facilitators through a rigorous qualitative research approach. Such an endeavor is critical as it represents a pivotal step towards mitigating the persisting disparities in healthcare system. As a result of these challenges, individuals with SCIs often experience poor community participation, which, in turn, affects their quality of life or vice versa.7Certainly, community inclusion is an important outcome to evaluate those who pursue the rehabilitation after SCI.8Therefore the present work was based on the objective to explore the barriers faced by SCI individuals after one of injury. It is also important to document about the facilitators which help in overcoming these challenges.
Materials and Methods
The present study was designed using a qualitative research approach. Qualitative research is exploratory by which the investigator can understand participants’ opinions, feelings as well as beliefs on the area of study. The study participants were recruited from the Kusum Spine and Neuro Rehabilitation Center (KSNR), which specializes in the comprehensive rehabilitation of SCI patients, encompassing physical therapy, vocational training, psychosocial support, and a primary focus on enhancing the patient-provider relationship. The study was carried out between December 2021 to June 2022 and was a part of a bigger project where the sample size was calculated using nMaster 2.0 software. The sample size was 240 (calculated with 6% margin of error and response rate of 39% in SCI patients). Out of this total sample size (i.e. 240), only 71 participants provided substantial responses to open-ended questions regarding the challenges they face post-injury and were included in the final analysis. Data saturation was achieved after 71 interviews. Though all the questions were mandatory for all of the participants recruited in the study but those who failed to answer open-ended questions adequately or provided vague responses were excluded. During data collection, participants were more willing to respond to closed-ended questions related to their current status and demographic details, but they were less comfortable with open-ended questions. This reluctance may be attributed to various factors, including the emotional toll of discussing their experiences or the complexity of articulating their challenges and coping mechanisms. This observation underscores the importance of understanding the context and sensitivities involved in qualitative research with this specific group.
For the present study, we conducted interviews with 82 participants on open-ended questions. However, it is crucial to acknowledge that not all responses contributed equally to the present study analysis due to the complex nature of participants’ experiences. Eleven participants provided responses that did not directly address the posed questions; their answers were disjointed and did not offer specific insights into the challenges and facilitators related to community reintegration following SCI. These interviews, in a sense, deviated from the intended path, and their content could not be meaningfully incorporated into the final analysis. Upon careful evaluation of these eleven interviews, both research team members (MM & RD) collectively decided to include only the responses from the 71 participants who provided clear and relevant answers to the interview questions. This decision aimed to maintain the quality and focus of the research data analysis, emphasizing the challenges of conducting research within the SCI community, particularly through the qualitative research process.
Hence, only 71 SCI individuals were included in this study using purposive sampling. Inclusion criteria consisted of: 1) individuals who had sustained SCI (both traumatic and non-traumatic); 2) those living in the community with at least one year post-injury; 3) individuals who had been admitted to or had visited the KSNR healthcare center for rehabilitation; 4) individuals aged 18 years or older; 5) participants who were able to read, speak, and understand Hindi or English and who were conscious without severe cognitive impairment (as per medical records and history taking); 6) participants who responded to all open-ended questions. Excluded were participants who had declined to provide written consent, refused to answer open-ended questions, had co-morbidities like cognitive dysfunction, brain injury, amputation, or belonged to vulnerable participant groups unable to participate in the study.
Data collection involved face-to-face in-depth interviews with an open-ended questionnaire. To get further insight into the present status of the participants, few additional information was gathered through a questionnaire, including participants’ demographic details, any illnesses occurring in the past year (secondary complications), treatment received and unmet healthcare needs.
The interview questions were developed following a comprehensive review of current literature and incorporated three open-ended questions:
What are the factors which influences the challenges during community participation following SCI?
Do you think that some persons with SCI doing better than you? If yes why?
What do you think are the best ways to overcome these challenges faced by you during community participation?
The first question was designed to know more about participant’s daily obstacles and to engage them in discussion around the consequences after SCI. The second question focused on participants’ viewpoint towards other SCI individuals. However, the last question was about to discuss the coping mechanisms to rule out the challenges which arisen only after SCI.
The duration of the interviews ranged from 35 to 47 minutes. Interviews were held in a peaceful environment and no external person was allowed. Before initiating the data collection, all the required information was shared and explained to the respective participants’ such as Participant Information Sheet (PIS) which includes study’s purpose, method, duration, withdrawal, confidentiality information and contact information/s. The discussion rules were also clarified to all participants. Only those participants were recruited in the study who has given the signed Informed Consent Form (ICF). All the interviews were recorded and later transcribed into verbatim to avoid bias. Personal information of the participants were anonymized to maintain participant confidentiality, such as instead of ‘Name’, researcher used ‘Initials’. However, all demographic data was entered into SPSS version 23 and was later analyzed for frequency distribution and percentages. Whereas qualitative data were gathered and entered into excel and later codes as well as themes were generated. The MAXQDA 2020 was used to organize, code, and manage the data.
All interviews were subjected to a rigorous analysis using Braun and Clarke’s thematic analysis method, as illustrated in Figure 1. Thematic analysis is a systematic approach employed for examining both verbal and written communication by employing a coding and categorization methodology. This method is particularly well-suited for delving into individuals’ experiences and perceptions.9,10In this study, the analysis utilized inductive approach, as described by Braun and Clarke.11 Thematic analysis is a type of qualitative analysis that allows one to classify and present themes relevant to the data.11 Thematic analysis provides concise description and interpretation in terms of themes and patterns from a data set. Braun and Clarke recommended the six stages to conduct thematic analysis. Throughout the six stages, first to familiarize with the data followed by searching, reviewing, defining, naming, and writing themes. These steps help to complete the analysis (refer Figure 1). To ensure the rigor of the present qualitative study, the criteria introduced by Lincoln & Guba, including credibility, dependability, confirmability, and transferability, were employed to establish its trustworthiness.12,13 However, in the present study, both authors (MM and RD) independently conducted data coding after a thorough review/familiarization of transcripts from all interviews, focusing on segments relevant to the current research. Any disagreements were thoroughly discussed, leading to the subsequent organization of related codes into potential sub-themes and themes by both authors (MM and RD). Following this, both authors (MM and RD) collaboratively assessed the themes to ensure that (I) the codes within each theme were cohesive, and (II) the codes across different themes were distinctly identifiable. Ultimately, the authors defined and named the themes in consensus, and they collectively generated a narrative structure with accompanying explanations. All these themes were validated, reviewed, and agreed by the research team members (MM & RD). The MAXQDA 2020 was used to organize, code, and manage the data.
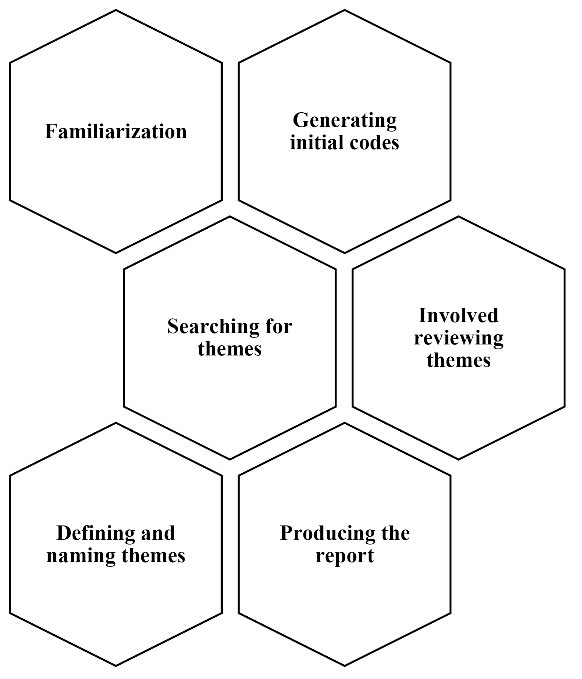
Figure 1.
Steps for thematic analysis
.
Steps for thematic analysis
This flowchart visually represents the process of conducting thematic analysis using Braun and Clarke’s 6-step Guide to Good Thematic Analysis framework.
Results
The response rate was 29.5% (71 of 240). The socio-demographic and clinical characteristics of the participants were listed in Table 1. Most of the participants were from the young age group i.e. 18-30 years. Participants consisted of 15 (21.1%) females with a mean age of 34.53 years (SD 14.8) and 56 (78.9%) males with a mean age of 32.75 years (SD 12.3). However, overall mean age of the study participants were 33.13 years with S.D 12.8. Majority of the study participants were from Delhi n=19 (26.8%) followed by Haryana, Uttar Pradesh n=18 (25.4%), n=15 (21.1%). There were maximum number of the participants were found to be graduate n=30 (42.3%). No participant was reported illiterate. Most of the participants reported that they ‘Daily’ go out from their home as their houses are on ground floor. In addition to this, half of the participants were reported unmarried n=46 (64.8%). Thoracic region was found to be the most common level of injury amongst the participants n=41 (57.7%). Whereas, road traffic accidents were commonest among all causes of injury followed by falls. Almost all participants reported secondary complications which includes, spasticity, urinary tract infection, pressure sores, pain etc. However, it was observed that maximum of the SCI individuals reported unmet healthcare needs after injury. Majority of the participants reported that poor finances and unawareness (neither patient knows about the injury and its consequences nor their care givers) were the primary reasons for their unmet healthcare needs (49.29% & 56.33%) followed by accessibility (i.e. transportation) (53.52%), no rehabilitation insurance (33.80%). In addition to this, COVID (40.08%) was also one of the biggest challenges among the SCI community (Table 2). In continuation to this, SCI participants prefer to choose ‘Home remedy’ case of any illnesses occurred after the injury due to their unmet needs. This might be the reason of the poor health seeking behaviour amongst the spinal cord injured community (Table 3).
Table 1.
Socio-demographic characteristics of participants with SCI (N=71)
|
Characteristics
|
No. (%)
|
| Age group (y)a |
|
| 18-30 |
40 (56.3) |
| 31-40 |
18 (25.4) |
| 41-50 |
7 (9.9) |
| 51-60 |
2 (2.8) |
| >61 |
4 (5.6) |
| Gender |
|
| Female |
15 (21.1) |
| Male |
56 (78.9) |
| Locality |
|
| Rural |
44 (62) |
| Urban |
27 (38) |
| Marital status |
|
| Married |
46 (64.8) |
| Unmarried |
24 (33.8) |
| Divorced/Separated |
1 (1.4) |
| Cause of injury |
|
| Sports |
1 (1.4) |
| Fall |
19 (26.8) |
| Assault |
3 (4.2) |
| Transport |
40 (56.3) |
| Non-traumatic |
8 (11.3) |
| Level of injury |
|
| Cervical |
17 (23.9) |
| Thoracic |
41 (57.7) |
| Lumbar |
7 (9.9) |
| Thoracolumbar |
6 (8.5) |
| Place of residence |
|
| Delhi |
19 (26.8) |
| Outside Delhi |
52 (73.2) |
| Education |
|
| Primary school certificate |
7 (9.9) |
| Middle school certificate |
3 (4.2) |
| High school certificate |
14 (19.7) |
| Intermediate or Diploma |
10 (14.1) |
| Graduate |
30 (42.3) |
| Profession or honors (postgraduate or above) |
7 (9.9) |
| Occupation |
|
| Unemployed |
45 (63.4) |
| Employed |
26 (36.6) |
| Income |
|
| Less than 10001 |
13 (18.3) |
| 10002–29972 |
16 (22.5) |
| 29973– 49961 |
14 (19.7) |
| 49962–74755 |
7 (9.9) |
| 74756 –99930 |
2 (2.8) |
| 99931–199861 |
11 (15.5) |
| Family type |
|
| Nuclear |
37 (52.1) |
| Joint |
34 (47.9) |
| Religion |
|
| Hindus |
62 (87.3) |
| Muslims |
4 (5.6) |
| Christians |
1 (1.4) |
| Sikhs |
3 (4.2) |
| Jains |
1 (1.4) |
| How frequent you go out from your home |
|
| Daily |
42 (59.2) |
| Sometimes |
15 (21.1) |
| Rarely |
14 (19.7) |
| Which floor do you live on |
|
| Ground floor |
55 (77.5) |
| 1st floor |
5 (7) |
| 2nd floor |
7 (9.9) |
| 3rd floor and above |
4 (5.6) |
a Mean (SD)=33. 13 (12.8).
Table 2.
Distribution of unmet healthcare needs (N=71)
|
|
Yes
|
No
|
| Financial |
35 (49.29) |
36 (50.70) |
| No insurance |
24 (33.80) |
47 (66.19) |
| Distance/transportation |
38 (53.52) |
33 (46.47) |
| No professional help |
27 (38.02) |
44 (61.97) |
| No support from family |
17 (23.94) |
54 (76.05) |
| Unawareness about the injury and its consequences |
40 (56.33) |
31 (43.66) |
| Ramifications of the coronavirus (COVID-19) outbreak |
29 (40.08) |
42 (59.15) |
Table 3.
Frequency distribution of illness occurred chosen treatment
|
|
No. (%)
|
| Present secondary complications |
|
| Gastrointestinal |
10 (14.08) |
| Spasticity |
12 (16.90) |
| Pain |
10 (14.08) |
| Urological |
07 (9.85) |
| Pressure Sores |
20 (28.16) |
| Others |
1 (1.40) |
| Did you suffer from any medical complication/s after the injury* |
|
| Yes |
66 (92.95) |
| No |
5 (7.04) |
| How the illness was treated |
|
| No illness reported |
4 (7.04) |
| Home remedy |
17 (23.94) |
| Ayurveda |
09 (12.67) |
| At hospital |
13 (18.30) |
| Faith healer |
10 (14.08) |
| I do not know |
3 (4.22) |
| Homeopathy |
9 (12.67) |
*Occurrence of any illnesses in past one year of data collection)
All the codes and sub-themes were merged into four major themes which were derived from the responses given by the participants (Figure 2). Exact phrases stated by some of the participants have been quoted in italics. The four major themes were further divided into several sub-themes specific to the single problem domain. The four major themes of barriers included environmental barriers, cultural barriers, psychological barriers and health-related barriers.
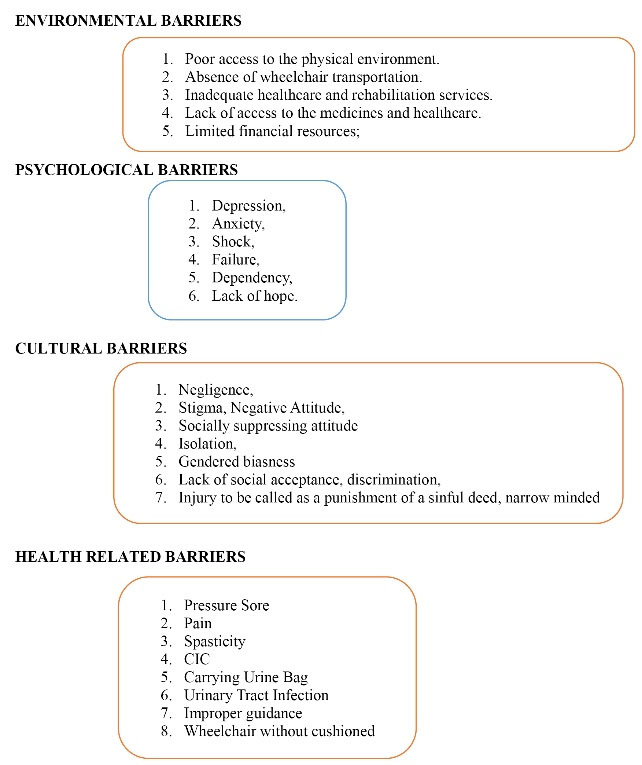
Figure 2.
Themes and sub-themes
.
Themes and sub-themes
Thematic Framework: Barriers to Community Integration in Spinal Cord Injury Patients
Environmental Barriers
A total of 57 participants (80.3%) reported environmental challenges while reintegrating into the community after the injury. Several sub-themes were extracted out from the participant’s responses which was perfectly merged into the major theme of Environmental issues. These sub-themes were poor accessibility, improper roads (uneven, muddy, narrow), slops and stairs, lack of assistance, crowded places, inappropriate wheelchairs, inadequate healthcare and rehabilitation services, no access to the medicines and healthcare especially in rural areas, limited financial resources, local transportation, need help at home or workplace, poor government policies, insurance issues were reported by the participants during their interview.
Inaccessible environmental structure such as no ramps, lifts especially at the public places are the vital factors and found to be the significant barrier for the SCI community. Even many participants reported they cannot go out for a walk alone on the wheelchair even after the five years of injury due to uneven, muddy roads. Almost all participants described their situations, where they were restricted from participating in community activities due to manmade barriers. In addition to that, most of the patients reported their unmet healthcare needs such as due to financial constraints, no insurances led them to poor quality of life as there were no proper rehabilitation and treatment plans.
Participant ‘11’ stated that:
“I got this injury long back, almost 5 years back… and I have shifted my house from second floor to ground floor. But still I have to request my family members to accompany me for a 10min walk because of uneven, broken roads. I feel so bad and helpless….”
Participant ‘16’ shared his response towards the challenges after SCI:
“I always love to visit places…I like travelling but unfortunately after this injury I am completely home bound… I am dependent on my family, friends…if they take me along with them...will always expensive at the places…affordable restaurants and hotels generally not have ramps... we are not so elite…. And I am unemployed too… so I prefer to stay back…”
Participant ‘2’ said:
“I wanted to start the rehabilitation after my discharge from the hospital… but there is no insurance coverage of outpatient/opd rehabilitation... I had no money that time… I have started my proper rehabilitation after 2 years of my injury. People like me are doing better than me … I think because of proper rehabilitation and exercises.”
Cultural Barriers
Most of the participants (n = 44, 62%) in this qualitative review were from urban regions. Cultural barriers were reported by 49.3% of the participants (n = 35). Negligence, stigma, attitude (negative or commiseration), language problem, isolation, gendered biasness, lack of social acceptance, discrimination, injury to be called as a punishment of a sinful deed, narrow minded were considered as sub-themes under cultural barriers. These all were mentioned in the responses of the participants during their interview.
Socially suppressing attitude is the key factor for cultural challenges. It includes compassionate attitude, disability attitude, inhuman attitude & atonement attitude.14 Participants of the present study mentioned about their bad experience with the society members and according to them that attitude pushes behind them to be a part of the community again.
Participant ‘21’ shared:
“I never prefer to go out… because whenever I go out with my family members for a walk or to buy my regular medicines… some or the other person starts staring at me... I remember a recent incidence with me… I went out with my father to buy my medicines… at the shop one lady came and suddenly started staring at me with gloomy eyes and a sense of compassion… she said, oh my god... how sad... pity for you… you are quite young... how old are you... you cannot do anything now… God please help her...”
Similarly, participant ‘6’ stated:
“I am living in a rural place… my neighbors always talk about me... they asked my parents that what I did in the past or in my past births…any sinful deed... and this is the punishment I got from the God… they said it is my ‘Karma’”
“I cannot change this attitude that’s why I prefer not to be social with anyone.. I always stay in my room. And after a long time I come (here) out from my home only for the rehabilitation.”
Most of the participants actually emphasized on the point that compassionate and sympathized behavior made them feel low, depressed. Especially in the first few years of the injury, participants needs hope, determination, love, concern, holistic approach rather than pity on them.
Psychological Barriers
SCI usually demands considerable changes in the life of an individual, and their family members. This may demand difficult psychological adjustment and in addition place great strain on family roles and relationships. Glass summarizes the situation thus: “The experience of SCI is one of the most devastating injuries which might affect an individual. The resultant disability, after which normal cognitive function and intellectual ability usually remains, produces not only an inability to move and feel limbs, but also the inability to control the function of internal organs and even, in severe cases, the ability to breathe independently.”15,16
In the present study, we found half of the participants (n = 36, 50.7%) reported psychological barriers during their participation in the community after this devastating injury. However, during the interviews there were many participants who did not disclose their psychological challenges due to many reasons. The researchers were unable to report those which were clearly not stated by the participants. It can be assumed that almost all participants were suffering from psychological challenges or fighting with it to overcome from it.
Depression, anxiety, shock, failure, dependency on others, lack of hope, separation from spouse/family members, inability to sleep, no social contacts, dissatisfaction, and loneliness were the sub-themes found under the umbrella of psychological barriers.
There are many instances shared by the spinal cord injured participants that no social network, change in family/friends behaviors put them in depression and anxiety.
Participant ‘13’ stated:
“I was doing my Engineering when I met with an accident… I was in a relationship for last 5 years…. And just after the injury my life …emotions… everything has changed… that girl left me by saying that their parents will not allow her to meet with me…”
“I never demanded anything… I just need friends to talk… I am all alone now… this always pushing me to this tragic event and I am not able to come out of it… I usually take medicines which help me to sleep.”
Health-Related Barriers
A total of 60 participants (84.5%) reported experiencing secondary health conditions that affected their community participation. Key factors limiting mobility and interest included pressure sores, urinary tract infections, and pain, followed by spasticity and bowel issues. Specifically, 28.16% of participants reported having pressure sores, followed by spasticity (16.90%), pain (14.08%), and gastrointestinal disease (14.08%).
Insufficient awareness and inadequate medical treatment, such as the lack of knowledge about performing clean intermittent catheterization (CIC) and managing issues like bed sores and urinary tract infections, hindered their social participation and diminished their confidence. Participants in the present study provided information on these challenges.
Participant ‘8’ stated:
“I do not prefer to meet people… going back in the community again is a big challenge for me... carrying a urine bag with me... stick to my wheelchair... people ask me what I am carrying it with me... making fun at times... my life has changed… and it is impossible... that society will accept me like this...”
Facilitators
During the interview, question number 3 was based on to know the factors which influence the SCI individuals to overcome form this life-altering event. Most of the participants responded that support from the family is the significant determinant to overcome from the trauma.
Following are the categories were derived from the responses of the SCI participants: 1- Family support; 2- Financial stability; 3- Religious practices; 4-Friends and leisure activity
The findings stated that 40.8% of the participants said family support was the most significant factor followed by financial stability, religious practices and friends and leisure activity (26.7%, 21.1%, & 11.2%). Most of the study participants answered this question without mentioning any such details. They expressed happiness that their families understand their injury and its consequences and do not judge them. However, financial concerns were raised by most of the participants. They felt that addressing these concerns could significantly improve their lives and serve as a major facilitator in overcoming the present challenges, especially those related to seeking treatment, rehabilitation, and transportation. However, there was only one participant who shared their experiences in detail in this section:
Participant ‘8’ stated:
Participant number 8 shared their experience about how strange it was for him to carry a urine bag and face the world.While discussing this challenge in their life, he mentioned, “I am still apprehensive about facing the community, but my parents and family members, especially my younger sister, were so supportive and enthusiastic that she never made me feel like I am on a wheelchair … and that my bodily appearance has completely changed.”
“Her discussion on the matter, her positive attitude, and her awareness about the subject made me feel comfortable in my home…. This, in turn, had a positive impact on me, and I am hopeful that I will gradually gather the courage to confront this harsh reality...and face the world … my community….””
However, these key facilitators that individuals with SCI can harness to overcome challenges and improve their quality of life. These are instrumental in aiding their rehabilitation journey and enhancing their community participation.
It is also noteworthy to mention that participants in the study reported a strong preference for utilizing the facilities provided by faith healers during their illnesses, as it offers them emotional and spiritual support. However, in this study, 14.08% of the SCI participants preferred visiting ‘faith healers’ instead of proper hospitals during their illnesses.
Discussion
The present study described the challenges faced by the SCI individuals during their community participation. It is very difficult for them to reintegrate into the society due to numerous barriers. Each age group has their own set of challenges and some of them are trying very hard to overcome those by finding different ways and means. Few of the participants have accepted their present bodily appearance after the injury whereas many are still struggling to accept the truth. Thus far, to our knowledge very limited studies have been published which mentioned about the challenges and facilitators faced by the SCI individuals from a low middle income country. Our work further reinforces the importance of employment, family, awareness as well as motivational talks which help the SCI individuals to participate in the community fully without any inferiority complex. It is imperative to know that the present study findings yielded enormous evidence reporting that physical environmental factors (such as access to public places, public transport, financial constraints, and unemployment) and secondary health conditions are the major deterrents for the SCI people to reintegrate into the community. Dorjbal et al conducted an explorative qualitative study in Mongolia with an aim to explore the experiences of SCI individuals. The findings were focused on the environmental barriers which was the main reason for the development of secondary health conditions, restricted activities, and participation in almost all areas of life.17 Various studies emphasized that fact that people with sustained SCI often use healthcare services as compared to people without disabilities due to their secondary complications such as sepsis, pressure ulcers, and urinary tract infection,18,19 and due to this their quality of life majorly affected.20,21 Likewise, Hossain et al conducted a mixed retrospective-prospective cohort design to determine survival after SCI in low- and middle-income countries like Bangladesh. Findings of the study supported that cushions on wheelchairs and foam overlays on beds would help prevent the deaths amongst SCI individuals due to sepsis and pressure ulcers.22 However, in the present study participant’s complaint of poor- quality wheelchair which was either donated by some of the organization or self. Most of the participants’ family income was poor and their socio-economic status was found to be ‘lower’ or ‘upper lower’ class. They cannot afford to have a costly comfortable wheelchair.
Furthermore, with the help of present study’s findings, revealed the interrelationship between the barriers reported by the participants during the interview. If a person gets an appropriate healthcare facility, including appropriate wheelchairs, walkable roads, and affordable/accessible local transportation for mobility, he or she is unlikely to bother about other obstacles such as societal attitude which triggers psychological issues. Environmental constraints mainly cause discrimination and a lack of confidence in SCI population, leaving them completely reliant on their caregivers.17,23 A cross-sectional study was conducted by Müller et al author concluded that those SCI individuals with better social support took lower scores in depression and higher scores in quality of life.7,24 If the quality of life elevated, it is a positive sign of improvement in overall personality of the SCI individual. United Nations stressed on the significance of accessibility for disabled individuals and primarily working on to promote how to engage disabled community in social activities and re-integrated into the society.25,26 But, in low- and middle-income countries, limited transportation, mobility, and social impediments are the primary deterrents for SCI people’s community inclusion. Studies indicated that unemployment rates are 10 times higher among SCI patients compared with the general population.27-30 Access to the place of work, employer attitudes, and patients’ beliefs in their abilities may influence the decision to resume employment after SCI. Singh et al found that employment status was associated with a higher QoL among those with SCI living in India.31 Moreover, government policies, particularly social policies, significantly impact the participation of SCI people with physical disabilities.29,32 Social support, education level, financial standing, job security, and involvement in social and recreational activities have all been identified as factors that may affect a person’s ability to adjust to SCI.
The present work also painted the facilitators that influence the SCI people to overcome from the emotional and may be from the physical obstacles. These variables positively worked on individuals’ life and boost them to reintegrate into the community ‘fully’. A similar work on facilitators was done by Xue et al in 2016. Through his cross-sectional questionnaire based study, he conveyed the importance of the rehabilitative programs which support patients’ spirituality/religiosity activities and mental wellbeing.33 A similar study based on a focus group research design examined the coping mechanism after SCI. The findings suggested that family support as well as spiritual practices provided solace, consolation, and inner quiet to participants, especially during difficult times, helping them participate in community activities, build confidence.34 Family support provides a fundamental role in both depression and adjustment to new life in SCI individuals. Persons who enjoy and involve more socially either in family or friends, they improve faster and easily accept the cruelty of life. They are less emotionally distressed and report better life satisfaction and improved quality of life.35
Conclusion
In conclusion, accessibility to the local transportation, public toilets, unemployment, limited financial resources, negative attitude and depression were found to be the major obstacles for SCI individuals from participating in the community. Most of the studies underlined the key factors that are the broader term for these above-mentioned barriers, such as acceptability, affordability, and accessibility. Furthermore, coping strategies/facilitators such as spirituality/religiosity and family/friends support are essential for SCI people to reintegrate into the community fully. Barriers becomes the weaknesses and facilitators are the strengths of the SCI individuals. People with SCI and their caregivers (family members) should count be an important part of the rehabilitation team so that they understand the exercise planner, shifting procedure from bed to wheelchair, toileting methods etc. This will help them to understand the injury and its consequences and due to their support, the psychological burden amongst the SCI individuals can be controlled. Healthcare professionals could strengthen the patient-provider interaction by establishing short- and long-term treatment goals such as independence, vocational training, a positive attitude, and counseling-spousal involvement, considering patients’ clinical and demographic variables. Working on the abovementioned issues can help SCI people in low- and middle-income countries become more integrated into their communities.
coi-Statement
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. The data are not openly available to maintain the confidentiality and privacy of SCI research participants.
Ethical Approval
There were no ethical issues. The study was approved by Institutional Ethics Committee (IEC) of Indian Spinal Injuries Center, Reference number: ISIC/RP/2020/15. Written informed consent was taken from the participants to ensure their willingness to participate in the study.
Research Highlights
What is the current knowledge?
-
After completing the in-patient hospital services (i.e. rehabilitation), persons with spinal cord injury (SCI) return to their community with rudimentary knowledge and skills of integrating the livelihood situation. Living with a SCI is challenging, especially in a developing nation i.e. India, people with SCI confront various types of barriers and inaccessibility in their society.
What is new here?
-
This study comprehends the multispectral experience of barriers & inaccessibility during community reintegration of people with SCI. They had residual disabilities, and secondary complications and confronted numerous barriers.
-
However, the present study indicated the importance of providing appropriate interventions such as vocational rehabilitation support and strengthening the patient-provider interaction which will not only help enhance resilience among SCI people but will also aid in their effective reintegration and equal participation in society.
-
It is critically important to study and evaluate SCI person’s life perceptions and experiences in different cultural and social contexts so that their needs and challenges can be appropriately determined.
References
- World Health Organization (WHO). International Perspectives on Spinal Cord Injury [Internet]. Available from: https://www.who.int/publications/i/item/international-perspectives-on-spinal-cord-injury. Accessed November 10, 2021.
- Lines LM, Lepore M, Wiener JM. Patient-centered, person-centered, and person-directed care: they are not the same. Med Care 2015; 53(7):561-3. doi: 10.1097/mlr.0000000000000387 [Crossref] [ Google Scholar]
- Carr JJ, Kendall MB, Amsters DI, Pershouse KJ, Kuipers P, Buettner P. Community participation for individuals with spinal cord injury living in Queensland, Australia. Spinal Cord 2017; 55(2):192-7. doi: 10.1038/sc.2016.169 [Crossref] [ Google Scholar]
- Balint E. The possibilities of patient-centered medicine. J R Coll Gen Pract 1969; 17(82):269-76. [ Google Scholar]
- Mohan M, Deb R. Barriers and facilitators of community integration of people with spinal cord injuries living in low and middle-income countries: a systematic review. Func Disabil J 2022; 5(1):1-19. doi: 10.32598/fdj.5.50 [Crossref] [ Google Scholar]
- Burns AS, O’Connell C. The challenge of spinal cord injury care in the developing world. J Spinal Cord Med 2012; 35(1):3-8. doi: 10.1179/2045772311y.0000000043 [Crossref] [ Google Scholar]
- Darain H, Ullah I, Dildar M, Ibrar M. Long-term challenges to patients with spinal cord injuries. Phys Med Rehabil Kurortmed 2017; 27(3):160-3. doi: 10.1055/s-0043-104053 [Crossref] [ Google Scholar]
- Mohan M, Singh VV, Deb R. Relational empathy, holistic care, and quality of life in persons with spinal cord injuries: a cross-sectional study. Am J Phys Med Rehabil 2023; 102(11):1000-7. doi: 10.1097/phm.0000000000002261 [Crossref] [ Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24(2):105-12. doi: 10.1016/j.nedt.2003.10.001 [Crossref] [ Google Scholar]
- Kooranian F, ParsaYekta Z, Rassouli M. Barriers and challenges to self-care among older adults with knee osteoarthritis: a qualitative study. Ethiop J Health Sci 2022; 32(5):963-74. doi: 10.4314/ejhs.v32i5.12 [Crossref] [ Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3(2):77-101. doi: 10.1191/1478088706qp063oa [Crossref] [ Google Scholar]
- Johnson JL, Adkins D, Chauvin S. A review of the quality indicators of rigor in qualitative research. Am J Pharm Educ 2020; 84(1):7120. doi: 10.5688/ajpe7120 [Crossref] [ Google Scholar]
- Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Directions for Program Evaluation 1986; 1986(30):73-84. doi: 10.1002/ev.1427 [Crossref] [ Google Scholar]
- Hosseinigolafshani Z, Abedi H, Ahmadi F. What are the people's attitudes toward spinal cord injury victims (from common to elite). Iran J Nurs Midwifery Res 2014; 19(3):266-272. [ Google Scholar]
- Glass CA. Applying functional analysis to psychological rehabilitation following spinal cord injury. J Am Paraplegia Soc 1992; 15(3):187-193. doi: 10.1080/01952307.1992.11735872 [Crossref] [ Google Scholar]
- North North, N N. The psychological effects of spinal cord injury: a review. Spinal Cord 1999; 37:671-679. doi: 10.1038/sj.sc.3100913 [Crossref] [ Google Scholar]
- Dorjbal D, Prodinger B, Zanini C, Avirmed B, Stucki G, Rubinelli S. Living with spinal cord injury in Mongolia: a qualitative study on perceived environmental barriers. J Spinal Cord Med 2020; 43(4):518-31. doi: 10.1080/10790268.2019.1565707 [Crossref] [ Google Scholar]
- Øderud T. Surviving spinal cord injury in low income countries. Afr J Disabil 2014; 3(2):80. doi: 10.4102/ajod.v3i2.80 [Crossref] [ Google Scholar]
- Gemperli A, Ronca E, Scheel-Sailer A, Koch HG, Brach M, Trezzini B. Health care utilization in persons with spinal cord injury: part 1-outpatient services. Spinal Cord 2017; 55(9):823-7. doi: 10.1038/sc.2017.44 [Crossref] [ Google Scholar]
- Singh G, Prakash R, Bhatti VK, Mahen A. Spinal cord injury in organizational setup - a hospital based descriptive study. J Mar Med Soc 2019; 21(1):46-50. doi: 10.4103/jmms.jmms_67_18 [Crossref] [ Google Scholar]
- Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord 2013; 51(12):882-92. doi: 10.1038/sc.2013.112 [Crossref] [ Google Scholar]
- Hossain MS, Rahman MA, Bowden JL, Quadir MM, Herbert RD, Harvey LA. Psychological and socioeconomic status, complications and quality of life in people with spinal cord injuries after discharge from hospital in Bangladesh: a cohort study. Spinal Cord 2016; 54(6):483-9. doi: 10.1038/sc.2015.179 [Crossref] [ Google Scholar]
- Hammel J, Magasi S, Heinemann A, Gray DB, Stark S, Kisala P. Environmental barriers and supports to everyday participation: a qualitative insider perspective from people with disabilities. Arch Phys Med Rehabil 2015; 96(4):578-88. doi: 10.1016/j.apmr.2014.12.008 [Crossref] [ Google Scholar]
- Müller R, Peter C, Cieza A, Post MW, Van Leeuwen CM, Werner CS. Social skills: a resource for more social support, lower depression levels, higher quality of life, and participation in individuals with spinal cord injury? Arch Phys Med Rehabil 2015; 96(3): 447-55. a resource for more social support, lower depression levels, higher quality of life, and participation in individuals with spinal cord injury? Arch Phys Med Rehabil 2015; 96(3):a resource for more social support, lower depression levels, higher quality of life, and participat. doi: 10.1016/j.apmr.2014.09.006 [Crossref] [ Google Scholar]
- Whiteneck GG, Harrison-Felix CL, Mellick DC, Brooks CA, Charlifue SB, Gerhart KA. Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil 2004; 85(8):1324-35. doi: 10.1016/j.apmr.2003.09.027 [Crossref] [ Google Scholar]
- Hill H. Disability and accessibility in the library and information science literature: a content analysis. Libr Inf Sci Res 2013; 35(2):137-42. doi: 10.1016/j.lisr.2012.11.002 [Crossref] [ Google Scholar]
- Babamohamadi H, Negarandeh R, Dehghan-Nayeri N. Barriers to and facilitators of coping with spinal cord injury for Iranian patients: a qualitative study. Nurs Health Sci 2011; 13(2):207-15. doi: 10.1111/j.1442-2018.2011.00602.x [Crossref] [ Google Scholar]
- Scovil CY, Ranabhat MK, Craighead IB, Wee J. Follow-up study of spinal cord injured patients after discharge from inpatient rehabilitation in Nepal in 2007. Spinal Cord 2012; 50(3):232-7. doi: 10.1038/sc.2011.119 [Crossref] [ Google Scholar]
- Sekaran P, Vijayakumari F, Hariharan R, Zachariah K, Joseph SE, Kumar RK. Community reintegration of spinal cord-injured patients in rural south India. Spinal Cord 2010; 48(8):628-32. doi: 10.1038/sc.2010.6 [Crossref] [ Google Scholar]
- Carpenter C, Forwell SJ, Jongbloed LE, Backman CL. Community participation after spinal cord injury. Arch Phys Med Rehabil 2007; 88(4):427-33. doi: 10.1016/j.apmr.2006.12.043 [Crossref] [ Google Scholar]
- Singh R, Dhankar SS, Rohilla R. Quality of life of people with spinal cord injury in Northern India. Int J Rehabil Res 2008; 31(3):247-51. doi: 10.1097/MRR.0b013e3282fb7d25 [Crossref] [ Google Scholar]
- Irshad H, Mumtaz Z, Levay A. Long-term gendered consequences of permanent disabilities caused by the 2005 Pakistan earthquake. Disasters 2012; 36(3):452-64. doi: 10.1111/j.1467-7717.2011.01265.x [Crossref] [ Google Scholar]
- Xue S, Arya S, Embuldeniya A, Narammalage H, da Silva T, Williams S. Perceived functional impairment and spirituality/religiosity as predictors of depression in a Sri Lankan spinal cord injury patient population. Spinal Cord 2016; 54(12):1158-63. doi: 10.1038/sc.2016.56 [Crossref] [ Google Scholar]
- Arya S, Xue S, Embuldeniya A, Narammalage H, da Silva T, Williams S. Coping strategies used by traumatic spinal cord injury patients in Sri Lanka: a focus group study. Disabil Rehabil 2016; 38(20):2008-15. doi: 10.3109/09638288.2015.1111433 [Crossref] [ Google Scholar]
- Samuelkamaleshkumar S, Radhika S, Cherian B, Elango A, Winrose W, Suhany BT. Community reintegration in rehabilitated South Indian persons with spinal cord injury. Arch Phys Med Rehabil 2010; 91(7):1117-21. doi: 10.1016/j.apmr.2010.04.005 [Crossref] [ Google Scholar]