Journal of caring sciences. 12(4):228-234.
doi: 10.34172/jcs.2023.31959
Original Article
Psychometric Assessment of Infant Colic Scale in Iranian Population
Reihaneh Montazeri Data curation, Investigation, Writing – original draft, 1 
Shirin Hasanpour Conceptualization, Funding acquisition, Resources, Project administration, Writing – review & editing, 2, * 
Mojgan Mirghafourvand Methodology, Supervision, 3 
Mohammad Asghari Jafarabadi Formal analysis, 4, 5, 6 
Manizheh Mostafa Gharehbaghi Project administration, 7 
Soheila Bani Validation, Visualization, 2 
Author information:
1Student Research Committee, Department of Midwifery, Nursing and Midwifery Faculty, Tabriz University of Medical Sciences, Tabriz, Iran
2Physical Medicine and Rehabilitation Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
3Social Determinants of Health Research Center, Department of Midwifery, Nursing and Midwifery Faculty, Tabriz University of Medical Sciences, Tabriz, Iran
4Cabrini Research, Cabrini Health, VIC 3144, Australia
5School of Public Health and Preventative Medicine, Faculty of Medicine, Nursing and Health Sciences, Monash University, VIC 3800, Australia
6Road Traffic Injury Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
7Pediatric Health Research Center, Department of Pediatrics and Neonatology, Tabriz University of Medical Sciences, Tabriz, Iran
Abstract
Introduction:
Infant colic, causing excessive crying, poses anxiety for parents and a challenge for pediatricians and nurses. The Infant Colic Scale (ICS) serves to assess the severity and causal factors of colic. Despite its significance, the psychometric properties of ICS have not been evaluated in the Iranian population. This study seeks to address this gap by assessing the psychometric properties of ICS in Iran.
Methods:
A sample of 220 mothers with 2–16-week-old term infants diagnosed with infantile colic was selected through convenience sampling. Following forward and back-translation, the face validity, content validity, and construct validity of ICS were systematically evaluated. Reliability was examined through both internal consistency (Cronbach’s alpha) and test-retest stability methods.
Results:
Content validity index (CVI) and content validity ratio (CVR) values for ICS were 0.94 and 0.81, respectively. The good fit indices confirmed the validity of the five-factor structure. Cronbach’s alpha coefficient and intraclass correlation coefficient (ICC) were 0.71 and 0.94, respectively.
Conclusion:
The Persian version of ICS is a valid and reliable tool, suitable for assessing infantile colic in the Iranian population. Future studies and clinical practice can utilize this tool to identify major causes of this disorder in the Iranian context.
Keywords: Infant, Colic, Psychometric, Iran
Copyright and License Information
© 2023 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
The project was financed by Tabriz University of Medical Sciences (Grant No. 64083). The funding was spent on sampling and conducting the study
Introduction
Crying is the first essential behavior that infants exhibit to communicate their needs to their caregivers. However, it is sometimes difficult to find out the cause of crying. Excessive crying is a source of anxiety for parents and a challenge for pediatricians.1 Colic is a common disturbing functional disorder affecting the gastrointestinal tract of infants. It is a behavioral manifestation in 1-4-months-old infants that often results in excessive crying and restlessness.2,3 The prevalence of colic was reported to be 2%-73% worldwide.3,4 In Iran, a prevalence rate of 20% was reported in 2008,5 no new statistics on the disorder are available in Iran.
Typical symptoms of infantile colic include excessive crying, legs drawn up towards the abdomen, arched back, stretched legs, and flushed face. It peaks at around 5-8 weeks of age, and improves automatically at around 4 months of age. Three diagnostic signs of colic include crying that begins and ends for no apparent reason, lasts at least three hours a day, three days a week, and three weeks a month (Wessel’s criteria), with no evidence of faltering growth.3,6
Although the pathogenesis of colic is unclear, it is assumed to be associated with changes in intestinal micro flora and intestinal hormones, excessive gas formation, allergy to cow’s milk protein, behavioral problems (e.g. family tension and parental anxiety), old age of mother, birth status, maternal smoking, etc.7
Colic is diagnosed via clinical examinations and laboratory interventions are not recommended at all.8 Once diagnosed with colic, an infant should be followed up by a physician regularly until complete recovery. Researchers suggest that reassuring parents (that the problem will be resolved by 3-4 months of age without any serious long-term effect), providing social support, and reducing stress levels are the most effective ways to manage infantile colic.9
The assessment of colic is quite complicated. Given the ambiguous nature of colic, only a few tools have been made for the assessment and diagnosis of this disorder. Even the existing tools and scales have several limitations. Almost all of these tools focus merely on the criterion of “crying”, which cannot be used to define “colic”, although it is an important clinical feature.10 The Crying Diary Scale is among the most popular clinical tools used for diagnosing colic, in which parents need to record an infant’s fussy behaviors and duration of crying for 24 hours.11 The Crying Pattern Questionnaire is a simple form of the Crying Diary Scale,12 and the Infant Breastfeeding Assessment Tool evaluates the effectiveness of breastfeeding.13 Finally, the Infant Colic Scale (ICS) is the most effective but less popular questionnaire used for etiological diagnosis of colic in infants.14 ICS can assess causal factors of colic, although its diagnostic scope may be limited.10 No researcher has so far validated the ICS in Iran. This 22-item scale has five subscales including cow’s milk/soy protein allergy/intolerance, immaturity of the gastrointestinal system, immaturity of the central nervous system, difficult infant temperament, parent-infant interaction and problem infant. The items are scored on a six-point Likert scale.14
The criteria that define colic are unclear; however, the diagnosis of colic and the determination of colic factors are important in selecting interventions that can alleviate the infant’s symptoms.This tool (ICS) evaluates both the severity and the factors that cause colic. Considering that the ICS has not been psychometric assessed in Iran so far, this study aimed to assess the psychometric properties of ICS in Iranian population.
Materials and Methods
Inclusion criteria of participants were women with term infants from 2 to 16 weeks, diagnosis of infant colic based on Wessel criteria and confirmed by a pediatrician and exclusive breastfeeding of the infant. Exclusion criteria were SGA (small for gestational age) or LGA (large for gestational age) infants and infants with abnormality.
The minimum sample size for factor analysis is 10 people per item,15 and ICS has 22 items; thus, the sample size was determined as 220.
The necessary data were collected using the Infant Colic Scale (ICS) developed by Ellett et al. It includes the subscales of cow’s milk/soy protein allergy/intolerance (items 1-2), immaturity of the gastrointestinal system (items 3-6), immaturity of the central nervous system (items 7-14), difficult infant temperament (items 15-18), parent-infant interaction (item 19) and problem infant (items 20-22). These 22 items are scored on a six-point Likert scale including strongly agree (score 6), moderately agree (score 5), slightly agree (score 4), slightly disagree (score 3), moderately disagree (score 2), and strongly disagree (score 1). The total score ranges from 22 to 132 with higher scores indicating an increase in gas formation. Ellett et al confirmed the validity and reliability of the tool in 2002. In this study, Cronbach’s alpha value of all items was calculated as 0.73.14
The Socio-Demographic and Obstetric Questionnaire consisted of items such as mother’s age, spouse’s age, educational qualifications, job status, income status, number of pregnancies, number and type of deliveries, etc.
After obtaining permission from the designers of the ICS, the original version of the tool was translated from English into Persian by a native English speaker who was also fluent in Persian language. The researchers reviewed the new version of the scale, which was later translated back from Persian into English by two professional translators who had not participated in the previous phase. The final scale was prepared after two experts who were familiar with relevant specialized terms and were fluent in both languages reviewed the previous version of the tool.
The researcher visited three health centers in Tehran and used convenience sampling to enroll mothers of infants who met the aforementioned inclusion criteria from April 2021 to October 2021. The participants were informed about the research objectives and method, and those who were willing to participate in the study signed informed consent forms. Finally, the Socio-Demographic and Obstetric Questionnaire and ICS were completed by interviewing the participants.
Statistical analysis was performed using SPSS version 13 and Amos version 13. Normality of the distribution of the ICS items was assessed before analyses by the Kolmogorov-Smirnov test and all items had normal distribution.
To assess the face validity of the scale, 30 randomly selected eligible mothers were asked to rate all items in terms of difficulty, relevance, and ambiguity. Using a four-point Likert scale, the responses were scored from 1 (completely difficult/irrelevant/ambiguous) to 4 (completely simple/relevant/unambiguous). The following formula was used for calculating the impact score of each item:
Impact Score=Frequency (%)×Importance
(Frequency: The percentage of mothers who gave the same score to each item; Importance: The score given by mothers to each item)
An impact score>1.5 was considered acceptable for each item.
Qualitative and quantitative methods were adopted to assess the content validity of ICS. In the qualitative assessment phase, ten experts specializing in midwifery and neonatology were asked to review the items and provide corrective comments on the use of correct vocabulary and grammar, proper placement of items, and proper scoring. In the quantitative phase, the content validity ratio (CVR) and content validity index (CVI) were used to assess the scale. To calculate CVR values, the experts were asked to determine the necessity of each item using a four-point scale (including useless, unnecessary, useful, and necessary). A four-point Likert scale was also used to calculate CVI values based on the relevance, unambiguity, and simplicity of each item.
The construct validity of the scale was assessed using the confirmatory factor analysis (CFA). In addition, the exploratory factor analysis (EFA) was performed using the Kaiser-Meyer-Olkin (KMO) test and Bartlett’s test of Sphericity, and Eigenvalues and scree plot were used to determine the number of factors.
Factor analysis analyzes inner-variable relations, and extracts classes of items that are closely related to each other. In factor analysis, items with factor loadings < 0.3 are omitted, and the researchers decide whether to omit those with factor loadings between 0.3 and 0.5.16 The researchers then examine the consistency of the extracted factor and items with the dimensions of the main scale (ICS).
Confirmatory Factor Analysis
CFA was performed to assess the structure of the extracted factors. For this purpose, the suitability of the exploratory research model was assessed using goodness of fit indices. The following values were considered acceptable: Root mean square error of approximation (RMSEA) < 0.08, Tucker-Lewis index (TLI) ≥ 0.95, and comparative fit index (CFI) ≥ 0.90, and χ2⁄df ratio < 5. In addition, the significance of model coefficient and correlation tests was examined in CFA.
The reliability of the scale was assessed using test-retest reliability and internal consistency. The test-retest reliability of each item and the whole scale was assessed by calculating intra-class correlation coefficients (ICC) for the 30 randomly selected mothers who completed the questionnaire twice at a two-week interval.
Internal consistency was also assessed for each item and for the whole scale using Cronbach’s alpha method.Cronbach’s alpha above 0.7 was acceptable.
Results
Participants’ Characteristics
In total, 220 participants were enrolled from April 2021 to October 2021. The mean (SD) age of the women was 29.2 (4.7) years and most of them (83.6%) were housewives. Table 1 shows other socio-demographic characteristics of the participants.
Table 1.
Characteristics of the study participants (N=220)
|
Variable
|
No. (%)
|
| Age (years)* |
29.2(4.7) |
|
Education
|
|
| Elementary |
3(1.4) |
| Secondary school |
5(2.3) |
| High school |
2(0.9) |
| Diploma |
47(21.4) |
| University |
163(74.1) |
|
Job
|
|
| Housewife |
184(83.6) |
| Employee |
36(16.4) |
|
Income
|
|
| Not at all sufficient |
23(10.5) |
| Relatively sufficient |
120(54.5) |
| Completely sufficient |
77(35.0) |
|
Life satisfaction
|
|
| Completely |
102(46.4) |
| Relatively |
110(50.0) |
| Unsatisfied |
8(3.6) |
|
Number of pregnancies
|
|
| 1 |
123(55.9) |
| 2-3 |
89(40.5) |
| 4 and more |
8(3.6) |
|
Number of children
|
|
| 1 |
147(66.8) |
| 2-3 |
73(33.2) |
|
Number of abortions
|
|
| 0 |
172(78.2) |
| 1-2 |
46(20.9) |
| 3 and more |
2(1.0) |
| Husband's age (year)* |
33.6(4.6) |
| Infant's age (day)* |
69.5(30.2) |
|
Husband's education
|
|
| Elementary |
3(1.4) |
| Secondary school |
5(2.3) |
| High school |
8(3.6) |
| Diploma |
64(29.1) |
| University |
140(63.6) |
|
Husband's job
|
|
| Self-employment |
117(53.2) |
| Employee |
58(26.4) |
| Worker |
44(20.0) |
| Jobless |
1(0.5) |
|
House status
|
|
| Personal |
110(50.0) |
| Rental |
78(35.5) |
| House of woman's parents |
8(3.7) |
| House of spouse's parents |
24(10.9) |
|
Number of stillbirths
|
|
| 0 |
216(98.2) |
| 1 |
4(1.8) |
|
Infant’s gender
|
|
| Female |
111(50.5) |
| Male |
109(49.5) |
*Statistically significant.
Face and Content Validity
All items were described as relevant, unambiguous, and simple, and their impact scores were all>1.5; thus, the face validity of the scale was confirmed. All items had acceptable CVI and CVR values. Moreover, CVR and CVI values obtained for the whole scale were 0.81 and 0.94, respectively.
Reliability
Cronbach’s alpha coefficient obtained for the whole scale was 0.71; therefore, the Persian version of ICS has an acceptable internal consistency. In addition, Cronbach’s alpha coefficients for the constructs of cow’s milk/soy protein allergy/intolerance, immaturity of the gastrointestinal system, immaturity of the central nervous system, difficult infant temperament, and parent-infant interaction with problem infant were 0.864, 0.396, 0.681, 0.697, and 0.735, respectively. Table 2 presents a comparison between Cronbach’s alpha values obtained for the Persian version of ICS and those of the original tool.
Table 2.
Cronbach’s alpha coefficient subscale scores comparing the Iranian sample and the original American sample
|
|
Iranian sample Cronbach’s alpha
|
Original sample Cronbach’s alpha
|
| Cow’s milk/soy protein allergy/intolerance |
0.86 |
0.91 |
| Immature gastrointestinal system |
0.40 |
0.45 |
| Immature central nervous system |
0.68 |
0.61 |
| Difficult infant temperament |
0.69 |
0.81 |
| Parent-infant interaction+Problem infant |
0.73 |
0.65 |
| Total scale |
0.71 |
0.73 |
Using the test-retest method, the whole scale’s ICC (95% CI) was calculated as 0.94 (0.85-0.96), while those of the constructs of cow’s milk/soy protein allergy/intolerance, immaturity of the gastrointestinal system, immaturity of the central nervous system, difficult infant temperament, parent-infant interaction, and problem infant were 0.93 (0.85-0.96), 0.91 (0.79-0.95), 0.96 (0.92-0.98), 0.92 (0.83-0.96), 0.83 (0.56-0.90), and 0.91 (0.79-0.95), respectively.
Factor Analysis
Regarding the EFA results, KMO value was calculated as 0.681, and Bartlett’s p-value was smaller than 0.001; therefore, the data were adequate for carrying out a scale-based EFA. Given the obtained eigenvalues, the 5-factor scale was confirmed with a total variance of 50.7%. The factors included cow’s milk/soy protein allergy/intolerance (2 items), immaturity of the gastrointestinal system (4 items), immaturity of the central nervous system (8 items), difficult infant temperament (4 items), and parent-infant interaction with problem infant (4 items). Factor loadings for items 10(Colic is not related to baby being tired), 11 (Infant eats at the same time every day), 13 (Infant is always in motion when awake), and 14 (Infant sleeps at different times every day) were smaller than 0.3; thus, these items were omitted. The item 5 (Baby vomits milk that looks like it did before it was drunk.), which had the lowest factor loading in immaturity of the gastrointestinal system subscale, was removed according to the opinion of the authors of the article (Table 3).
Table 3.
Factor loadings of the Infant Colic Scale (n=220)
|
Items
|
Factor 1
|
Factor 2
|
Factor 3
|
Factor 4
|
Factor 5
|
| 1- What Mom eats affects whether or not the baby has colic |
0.938 |
|
|
|
|
| 2- What Mom eats affects how bad the colic is |
0.938 |
|
|
|
|
| 3- Baby does not usually vomit |
|
0.670 |
|
|
|
| 4- Baby may still be vomiting when time for the next feeding |
|
0.781 |
|
|
|
| 5- Baby vomits milk that looks like it did before it was drunk |
|
0.382 |
|
|
|
| 6- Baby has no difficulty passing stool |
|
0.454 |
|
|
|
| 7- Baby is jittery |
|
|
0.640 |
|
|
| 8- Colic occurs when the baby has had a busy day |
|
|
0.355 |
|
|
| 9- Baby does not need to be rocked to sleep |
|
|
0.642 |
|
|
| 10- Colic is not related to baby being tired |
|
|
0.182 |
|
|
| 11- Baby eats at the same time every day |
|
|
-0.082 |
|
|
| 12- Baby can go to sleep by himself/herself |
|
|
0.784 |
|
|
| 13- Baby is always in motion when awake |
|
|
0.003 |
|
|
| 14- Baby sleeps at different times every day |
|
|
0.073 |
|
|
| 15- Baby is cranky most of the time |
|
|
|
0.735 |
|
| 16- Baby does not cry easily |
|
|
|
0.673 |
|
| 17- Baby is happy most of the time |
|
|
|
0.864 |
|
| 18- Baby waits calmly while I get the food ready |
|
|
|
0.619 |
|
| 19- When baby starts to fuss, nothing I do helps |
|
|
|
|
0.531 |
| 20- When the colic starts, I can soothe him/her |
|
|
|
|
0.820 |
| 21- When the colic starts, nothing I do helps. |
|
|
|
|
0.803 |
| 22- I can tell what baby wants when he/she starts to cry |
|
|
|
|
0.627 |
Regarding the CFA results, χ2⁄df ratio and RMSEA were obtained as 1.917 and 0.065, respectively; therefore, the model had a desirable validity. In addition, the research model fitted the data well, because goodness of fit indices of TLI, and CFI were all>0.9. Figure 1 shows a path diagram with standardized coefficients of CFA.
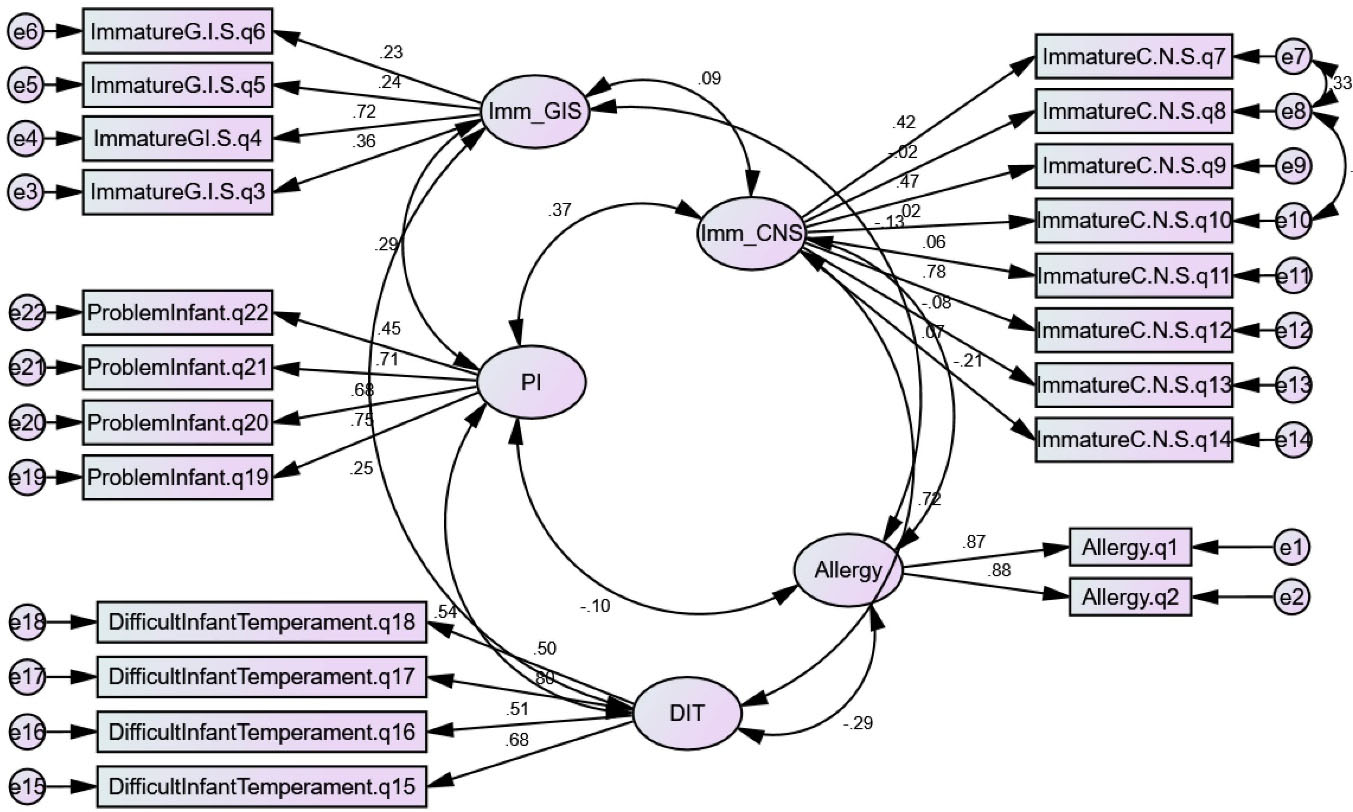
Figure 1.
CFA factor loading, a path diagram with standard coefficients of factor analysis
.
CFA factor loading, a path diagram with standard coefficients of factor analysis
Discussion
The results indicated that the Persian version of ICS is a reliable and valid tool for assessing infantile colic in Iranian population. The validity of the tool was confirmed using (quantitative and qualitative) face and content validity and construct validity. In addition, the reliability of the scale was assessed and confirmed using test-retest reliability and internal consistency (Cronbach’s alpha method). Therefore, the psychometric properties of the tool were all confirmed.
The obtained Cronbach’s alpha coefficient (0.71) indicated the acceptable internal consistency of the whole scale. Çetinkaya and Basbakkal calculated a Cronbach’s alpha coefficient of 0.73 for the Turkish version of the tool.17 In addition, the Cronbach’s alpha coefficients they obtained for the 5 subscales of ICS ranged from 0.55 to 0.89. In this study, an ICC of 0.94 was calculated for the whole scale indicating excellent reliability of the Persian version of ICS.
In EFA, about 50% of the variance of the 5-factor ICS was explained, which is acceptable in multidimensional tools.18 The obtained KMO value and Bartlett’s p-value confirmed the adequacy of the model. RMSEA was calculated as 0.065. In psychometric studies, RMSEA<0.08 indicates a good model fit; therefore, the overall model had a desirable model fit. Other goodness of fit indices also indicated a good model fit.
The face and content validity of the 5-factor ICS were desirable. This is in line with the findings of Çetinkaya and Basbakkal.17
Colic is a multifactorial phenomenon and its main cause is still unclear.14 Some possible causes of colic include gastrointestinal problems, parent-infant interaction problems, and immaturity of the central nervous system.14,19,20
In this study, items 10 (Colic is not related to baby being tired), 11 (Infant eats at the same time every day), 13 (Infant is always in motion when awake), and 14 (Infant sleeps at different times every day) were omitted, because their respective factor loadings were smaller than 0.3. The item 5(Baby vomits milk that looks like it did before it was drunk.), which had the lowest factor loading in gastrointestinal system subscale, was removed according to the opinion of the authors of the article. Çetinkaya and Basbakkal removed items 5, 6, and 11 from the original version of ICS, because their respective correlation coefficients were smaller than 0.3.17 Items 5 and 11 were omitted in both studies.
The Cronbach’s alpha coefficient obtained for the subscale of allergy/intolerance in the Persian version of the scale was very close to that calculated in the original tool. Cronbach’s alpha coefficients obtained for the subscales of immaturity of the gastrointestinal system, immaturity of the CNS, and difficult infant temperament in the Persian version of the scale were smaller than those calculated in the original tool. Finally, the Cronbach’s alpha coefficient obtained for the subscale of parent-infant interaction and problem infant in the Persian version of the scale was greater than that calculated in the original tool. The Cronbach’s alpha value obtained for the whole scale (0.71) was very close to that of the original ICS (0.73); therefore, the Persian version of ICS can be used in Iran for the same purposes as the original version.
This was the first study to assess the psychometric properties of ICS in Iran. However, the participants were selected using a non-random sampling method due to the COVID-19 pandemic.
Conclusion
As a valid and reliable tool, the Persian version of ICS can be used in future studies to assess infantile colic in Iranian population. Infantile colic is a source of anxiety for parents; therefore, researchers are recommended to identify major causes of this disorder using ICS.
Acknowledgments
The authors are grateful to the Research and Technology Deputy of Tabriz University of Medical Sciences, esteemed professors, personnel of the Health Centers of Tehran, participants, and other people who helped us in this study.
COI-statement
The authors declare that they have no competing interests.
Data Availability Statement
Data and materials of this study are available from the corresponding author upon reasonable request.
Ethical Approval
This study was conducted in accordance with the Helsinki Declaration and relevant guidelines. All participants were informed about the study and written informed consent was obtained from them. The Ethics Committee of Tabriz University of Medical Sciences confirmed the study (ethical code: IR.TBZMED.REC.1398.957).
Research Highlights
What is the current knowledge?
-
Colic is diagnosed via clinical examinations and the assessment of colic is quite complicated.
-
Infant Colic Scale (ICS) can assess severity and causal factors of colic, but ICS has not been psychometric assessed in Iran.
What is new here?
References
- Landgren K, Hallström I. Parents’ experience of living with a baby with infantile colic--a phenomenological hermeneutic study. Scand J Caring Sci 2011; 25(2):317-24. doi: 10.1111/j.1471-6712.2010.00829.x [Crossref] [ Google Scholar]
- Indrio F, Dargenio VN, Giordano P, Francavilla R. Preventing and treating colic. Adv Exp Med Biol 2019; 1125:49-56. doi: 10.1007/5584_2018_315 [Crossref] [ Google Scholar]
- Vandenplas Y, Hauser B, Salvatore S. Functional gastrointestinal disorders in infancy: impact on the health of the infant and family. Pediatr Gastroenterol Hepatol Nutr 2019; 22(3):207-16. doi: 10.5223/pghn.2019.22.3.207 [Crossref] [ Google Scholar]
- Vandenplas Y, Abkari A, Bellaiche M, Benninga M, Chouraqui JP, Çokura F. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr 2015; 61(5):531-7. doi: 10.1097/mpg.0000000000000949 [Crossref] [ Google Scholar]
- Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World J Gastroenterol 2008; 14(29):4662-6. doi: 10.3748/wjg.14.4662 [Crossref] [ Google Scholar]
- Wessel MA, Cobb JC, Jackson EB, Harris GS Jr, Detwiler AC. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 1954; 14(5):421-35. [ Google Scholar]
- Hirsh JL. Functional Analysis of Excessive Crying in Infancy: Two Empirical Case Studies. Western Michigan University; 2019.
- Türkoğlu Ünal E, Bülbül A, Kara Elitok G, Avşar H, Uslu S. Evaluation of the knowledge level and attitude of mothers about infantile colic. Haydarpaşa Numune Med J 2021; 61(1):38-4. doi: 10.14744/hnhj.2020.47135 [Crossref] [ Google Scholar]
- Fakhri B, Hasanpoor-Azghady SB, Amiri Farahani L, Haghani H. The relationship between social support and perceived stress in the mothers of infants with colic. Iran J Pediatr 2019; 29(1):e81353. doi: 10.5812/ijp.81353 [Crossref] [ Google Scholar]
- García Marqués S, Chillón Martínez R, González Zapata S, Rebollo Salas M, Jiménez Rejano JJ. Tools assessment and diagnosis to infant colic: a systematic review. Child Care Health Dev 2017; 43(4):481-8. doi: 10.1111/cch.12454 [Crossref] [ Google Scholar]
- Barr RG, Kramer MS, Leduc DG. Validation of a parental diary of infant cry/fuss behavior by a 24-hour voice-activated infant recording (VAR) system. Program Ambulatory Ped Association 1982;69.
- Wolke D, Meyer R, Gray P. Validity of the crying pattern questionnaire in a sample of excessively crying babies. J Reprod Infant Psychol 1994; 12(2):105-14. doi: 10.1080/02646839408408873 [Crossref] [ Google Scholar]
- Matthews MK. Developing an instrument to assess infant breastfeeding behaviour in the early neonatal period. Midwifery 1988; 4(4):154-65. doi: 10.1016/s0266-6138(88)80071-8 [Crossref] [ Google Scholar]
- Cirgin Ellett ML, Murphy D, Stroud L, Shelton RA, Sullivan A, Ellett SG. Development and psychometric testing of the infant colic scale. Gastroenterol Nurs 2003; 26(3):96-103. doi: 10.1097/00001610-200305000-00002 [Crossref] [ Google Scholar]
- Chou CH, Farn CK. Toward to measure narcissistic personality in cyberspace: validity and reliability. Psychology 2015; 6(15):1984-94. doi: 10.4236/psych.2015.615196 [Crossref] [ Google Scholar]
- O’Leary-Kelly SW, Vokurka RJ. The empirical assessment of construct validity. J Oper Manag 1998; 16(4):387-405. doi: 10.1016/s0272-6963(98)00020-5 [Crossref] [ Google Scholar]
- Çetinkaya B, Basbakkal Z. A validity and reliability study investigating the Turkish version of the Infant Colic Scale. Gastroenterol Nurs 2007; 30(2):84-90. doi: 10.1097/01.sga.0000267925.31803.30 [Crossref] [ Google Scholar]
- Büyüköztürk Ş. Faktör analizi: temel kavramlar ve ölçek geliştirmede kullanımı. Kuram ve Uygulamada Eğitim Yönetimi 2002; 32(32):470-83. [ Google Scholar]
- Zeevenhooven J, Browne PD, L’Hoir MP, de Weerth C, Benninga MA. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol 2018; 15(8):479-96. doi: 10.1038/s41575-018-0008-7 [Crossref] [ Google Scholar]
- Abbas ME. Diagnosis and management of infant colic. Am J Med Clin Res Rev 2023; 2(8):1-6. doi: 10.58372/2835-6276.1061 [Crossref] [ Google Scholar]