Journal of caring sciences. 12(4):213-220.
doi: 10.34172/jcs.2023.33005
Original Article
Effectiveness of Swallowing and Oral Care Interventions on Oral Intake and Salivary Flow of Patients Following Endotracheal Extubation at a Tertiary Care Center: A Randomized Controlled Trial
Sherill Ann Chacko Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Lakshmi Ramamoorthy Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, 1, * 
Anusha Cherian Methodology, Project administration, Validation, Visualization, Writing – review & editing, 1 
R Anusuya Formal analysis, Methodology, Project administration, Project administration, Validation, Visualization, 2 
HT Lalthanthuami Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Rani Subramaniyan Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing, 1 
Author information:
1College of Nursing, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India
2Department of Anaesthesiology and Critical Care, JIPMER, Pondicherry, India
Abstract
Introduction:
Endotracheal intubation and mechanical ventilation are the most frequently used life-sustaining interventions in critical care. Prolonged intubation can lead to post-extubation dysphagia, affecting the individual’s nutritional level and communication ability. Thereupon, this study aims to assess the effectiveness of swallowing and oral care interventions in resuming oral intake and increasing salivary flow in post-extubation patients.
Methods:
A randomized controlled trial was conducted in critical care units of a tertiary care setting, where 92 post-extubation patients who had undergone intubation for≥48 hours were enrolled. The intervention group received swallowing and oral interventions, including safe swallowing education (SSE), toothbrushing, salivary gland massage, oral cavity, and swallowing exercises. In contrast, the control group received standard oral care every 8th hour. Oral intake was assessed daily with the Functional Oral Intake Scale, and the salivary flow measurement was assessed with oral Schirmer’s test on the 1st, 3rd, and 7th day after extubation.
Results:
The baseline demographic and clinical characteristics showed that the groups were homogenous. The intervention group achieved total oral intake two days earlier than the control group. Findings also showed that the participants in the intervention group had a significant increase in salivary flow than in the control group on the 3rd and 7th days of the intervention.
Conclusion:
Swallowing and oral care interventions help post-extubation patients resume early oral intake and increase salivary flow after prolonged intubation. Hence, it improves the patient’s outcome toward a healthy life.
Keywords: Airway extubation, Dysphagia, Swallowing, Oral care, Endotracheal, Salivary flow
Copyright and License Information
© 2023 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
This study received intramural fund from Jawaharlal Institute of Postgraduate medical Education and Research, Puducherry, India.
Introduction
Endotracheal intubation and mechanical ventilation are critical care’s most frequently used life-sustaining interventions. But, clinical trials within the last decade have shown that mechanical ventilation can cause additional mortality in some critically ill patients by causing trauma directly to the oral cavity, larynx, pharynx, and temporomandibular joint, which could affect conventional functions like oral intake of food, salivary flow, and vocal production. These disruptions in normal operations cause discomfort and affect the individual’s nutritional level and ability to communicate effectively.1 This understanding has generated more interest in endotracheal intubation, mainly in strategies to improve this further.
Normal swallowing depends on a complex sequence of perfectly timed physiologic events, some co-occurring, others sequentially, that involve contractions of multiple oral-facial, pharyngeal, laryngeal, respiratory, and oesophageal muscles.2 To prevent aspiration, a bolus of food or fluid reaching the posterior oral cavity stimulates neuroreceptors that trigger respiratory muscles to halt respiration.3 These neatly coordinated events could be disturbed due to the introduction of an endotracheal tube (ETT).
Post-extubation dysphagia is the failure to properly transfer food and liquids from the buccal cavity to the stomach in patients undergoing prolonged endotracheal intubation. It is prevalent, affecting 61.7% within 48 hours post-extubation. Even though the participants did not have prior swallowing difficulties or known pathologies like stroke or neuromuscular deficits, 15.5% had persistent dysphagia and were feeding tube dependent during the post-extubation period.4 It can also cause poor quality of life,5,6 aspiration pneumonia7, longer ICU& hospital stay, and increased 90-day mortality; but unfortunately, the evidence for dysphagia treatment is limited.8 The post-extubation dysphagia insists health workers develop and practice some intensive solutions to reduce the incidence of post-extubation dysphagia.
A study conducted at The University of Colorado, Denver, revealed that a large number of patients with prolonged endotracheal intubation were suffering from post-extubation dysphagia, and they suggested that the development of post-extubation dysphagia was associated with poor patient outcomes and decreased quality of life.9 Though the effect of post-extubation dysphagia is frequently observed, few studies have observed interventions to resolve the problems. For many years, researchers have considered the possibility of swallowing rehabilitation, including oropharyngeal exercises and oral hygiene, to improve post-extubation dysphagia and thereby increase nutritional intake among critically ill patients. However, there is limited evidence on the clinical application of swallowing rehabilitation, especially the patients receiving prolonged mechanical ventilation. Hence, the findings of the study will be significantly effective in reducing post-extubation complication.
Swallowing and oral care interventions can be effective in managing the adverse effects of prolonged endotracheal intubation; So that early resuming of total oral intake for patients who had been successfully extubated after prolonged intubation can be achieved, which will indeed increase their quality of life too. Keeping this in mind, we implemented nurse-administered swallowing and oral care interventions (i.e., toothbrushing, salivary gland massage, oral cavity exercises, swallowing exercises, and safe swallowing education [SSE]) to assess the effectiveness of these interventions on oral intake resume and salivary flow of the patients following Endotracheal Extubation.
Material and Methods
Design and Setting
Using a randomized controlled trial design, data were collected from critical care units for 8 months (January – August 2022) from a tertiary care hospital in the public health sector of South India.
Sample Size and Sampling
Participants were selected using a convenience sampling technique. The sample size was estimated using the formula for the comparison of two independent means. By considering the minimum expected mean (SD) difference between control and intervention groups in time taken to resume total oral intake after extubation as 2 (3.25) days, the sample size was estimated to be 46 in each group at a 5% level of significance and 80% power.10 The inclusion criteria consist of post-extubation patients who were ≥ 18 years, expected to have undergone endotracheal intubation for ≥ 48 hours, on enteral feeding, and who can understand and speak English/ Tamil fluently. Whereas, patients with neuromuscular diseases, swallowing difficulty before intubation (e.g. mass in throat, laryngeal cancer), tracheostomy, or who were unable to follow instructions were excluded from the study.
Randomization
Allocation Concealment Mechanism
The allocation sequence was computer generated using permuted blocks of varying sizes (sizes of 4, 6 and 8) and it was placed in sequentially numbered and opaque envelopes.
Randomization Implementation
Allocation concealment was done by an independent statistician who is not involved in the recruitment of patients. Those envelopes were used by the researcher in enrolling the participants and assigning them into control and intervention groups. (Consort diagram: Figure 1).
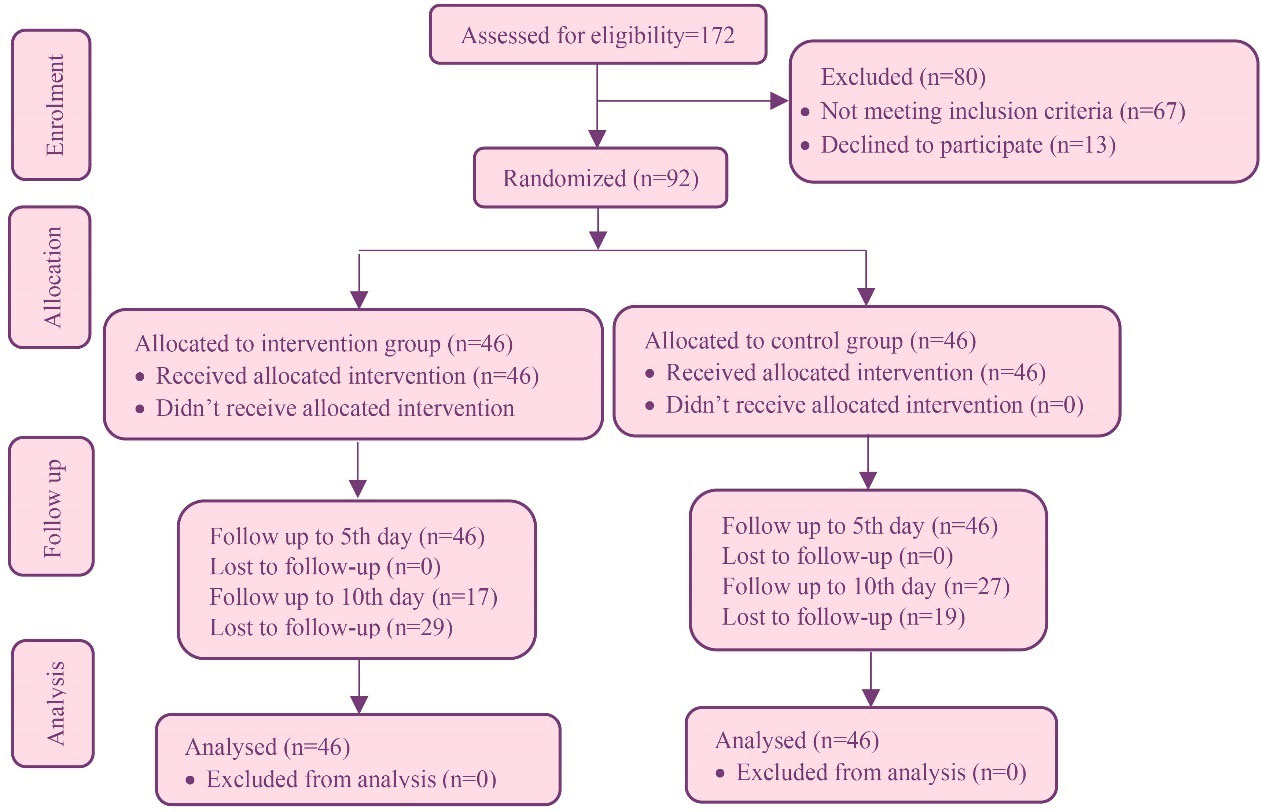
Figure 1.
Flowchart of the study
.
Flowchart of the study
Data Collection Instruments
Oral intake assessment using Functional Oral Intake Scale (FOIS): is a tool with established validity (81–98%) and inter-rater reliabilities (0.86 to 0.91) used for assessing the oral intake after extubation up to 14 days or up to discharge whatever occurs first. FOIS scores range from 1 to 7, with levels 1 indicating nothing by mouth (NPO), 2 to 3 indicating varying degrees of tube feeding, and levels 4 to 7 indicating varying degrees of oral intake.10
Salivary flow assessment with oral Schirmer’s test: The salivary flow will be evaluated 1st, 3rd, 7th, and 14th-day post-extubation using the oral Schirmer test. The subjects were not allowed to eat, brush or smoke for 2 hours 25 prior to the measurement. The participants were told to sit upright and instructed to swallow saliva. Schirmer’s tear test strip which is 1 cm wide by 35mm was placed at the floor of mouth.11
Intervention & Data Collection
For the control group: Upon extubation, standard care was provided wherein oral intake was withheld until participants demonstrated no signs of choking and then started with a small amount of water, progressing to small and consistent amounts of food/liquid as tolerated. Oral care is provided each shift by ICU nurses using oral swabs. Once patients are transferred to a general ward, oral care is considered a self-care process that will often be assisted by family members.
For intervention group: Upon extubation, the oral intake was withheld until participants demonstrated no signs of choking then swallowing, and oral care interventions10 were started including toothbrushing with distilled water using a soft toothbrush for 4 minutes, moisturizing their lips using Vaseline, gentle massage was given on the surface overlying the parotid, submandibular & sublingual salivary glands11 for four minutes, oral motor and swallowing exercises. Oral motor exercises12 include pursing the lips, cheek bloating, cheek sucking, lip protrusion, tongue protrusion, elevation, lowering and moving in different directions, and opening the mouth widely10 (each with 3, 5 or 10 repetitions with or without resistance, depending on the patient’s tolerance).
Swallowing exercises13 include Supraglottic swallow (airway protection exercise), in which the research nurse instructed the patient to hold their breath tightly then swallow saliva twice, and then release the breath with a sharp cough and swallow again. Masako exercise (base of tongue exercise), where the research nurse instructed the participant to stick out their tongue and hold it between lips or teeth and swallow saliva.
Shaker exercise (strap muscle exercise), in which the research nurse instructed the patient to lie down on their back without a pillow and by keeping the shoulders flat against the bed, lift the head and bring the chin down to the chest. Keep head lifted for 60 seconds and then lower head and rest for 60 seconds. SSE was given on the 1st day of intervention based on the intake status of the patient. The SSE consists of explaining signs and symptoms of unsafe swallowing, providing tips on sitting up to eat and modifying dietary texture and viscosity. The oral intake status of both the groups was assessed daily using FOIS for 10 days post-extubation, or until discharge, whatever happens first. FOIS scores 4 to 7 were considered as total oral intake in this study.10,14 The salivary flow of the participants was assessed by oral Schirmer’s test15 on the 1st, 3rd and 7th day of post-extubation and at the end of 5 minutes, a wetting length (in millimeters) was recorded. A large portion of the participants were lost for follow-up after the 5th day due to either re-intubation, discharge, or death of the patient.
Data Analysis
All the statistical analyses were done using IBM SPSS 13. The distribution of categorical variables such as gender, diagnosis, indication of intubation, etc. was expressed as frequency and percentages. The continuous data such as age, duration of intubation, FOIS score, salivary flow, etc. were expressed as mean with standard deviation or median with interquartile range (IQR). Comparison of baseline characteristics between the groups was done using the Chi-square test, Fisher’s exact test, Mann Whitney U test, and Independent Student t-test. The longitudinal change of salivary flow and oral intake status were compared between groups using Repeated Measures Analysis of Variance (RMANOVA) and Mann Whitney-U test respectively.
Results
The groups were homogeneous in age, nativity, and education. Regarding gender, male preponderance in the intervention group and female preponderance in the control group was noted (P<0.001). In terms of occupation employed participants are more in the control group (P<0.05).
The groups were similar in diagnosis and Acute Physiology and Chronic Health Evaluation )APACHE-II( score, a fraction of inhaled oxygen (FiO2), co-morbidities, an indication of intubation, and duration of intubation. Regarding smoking status, current smokers were more in the control group (P<0.05). The majority of the participants were intubated with 7.5-sized ETT in both groups; the participants who were intubated with size 8 ETT were more in the control group (P=0.042). Duration of intubation was greater in the intervention group (73.08 hours) as compared to the control group (64.12 hours), even though it was not statistically significant (P<0.207) (Table 1).
Table 1.
Comparison of baseline characteristics between intervention & control group (N=92)
|
Variable
|
Intervention (n=46)
|
Control (n=46)
|
P
value
|
| Age1 |
47.70 (15.88) |
52.20 (15.09) |
0.16a |
| Gender2 |
| Male |
44 (95.7) |
2 (4.3) |
<0.001*b |
| Female |
2 (4.3) |
44 (95.7) |
| Education2 |
| Uneducated |
2 (4.3) |
3 (6.5) |
0.88c |
| Elementary |
28 (60.9) |
29 (63.0) |
| High school and above |
16 (34.8) |
14 (30.4) |
| Diagnosis2 |
| Cardio-respiratory |
27 (58.7) |
22 (47.8) |
0.14 |
| Gastro-intestinal |
4 (8.7) |
5 (10.9) |
| Musculoskeletal |
5 (10.9) |
1 (2.2) |
| Others |
10 (21.7) |
18 (39.1) |
| APACHE-II score1 |
17.65 (6.32) |
18 (6.89) |
0.80 |
| FiO2 (%)3 |
| Day 1 (n=92) |
n=46 |
40.00 (0.00) |
n=46 |
40.00 (22.00) |
0.82 |
| Day 2 (n=51) |
n=26 |
28.00 (12.00) |
n=25 |
36.00 (12.00) |
0.43 |
| Smoking status2 |
| Current (n=29) |
10 (21.7) |
19 (41.3) |
<0.05 |
| Reformed (n=11) |
4 (8.7) |
7 (15.2) |
| Nil (n=52) |
32 (69.6) |
20 (43.5) |
| Comorbidities2 |
| Yes (n=56) |
30 (65.2) |
26 (56.5) |
0.39 |
| No (n=36) |
16 (34.8) |
20 (43.5) |
| Size of ETT (in mm)2 |
| 6.5 |
1 (100.0) |
0 (0) |
0.04 |
| 7 |
11 (73.3) |
4 (26.7) |
| 7.5 |
24 (52.2) |
22 (47.8) |
| 8 |
10 (33.3) |
20 (66.7) |
| Indication of Intubation2 |
| Respiratory distress |
21 (45.7) |
12 (26.1) |
0.15 |
| Altered sensorium |
7 (15.2) |
14 (30.4) |
| Hemodynamic instability |
1 (2.2) |
2 (4.3) |
| Surgery |
17 (37) |
18 (39.1) |
| Duration of intubation3 |
73.08 (98.56) |
64.12 (58.75) |
0.20 |
*Statistically significant, aP>0.05, bP<0.05, bP>0.05, *P value<0.05.
1
Mean (SD) & Independent student t-test; 2Frequency (%) & Chi-square test.
3
Median (interquartile range) and Mann-Whitney U test.
The mean difference in salivary flow between the groups on Day 7 of the intervention (7.56 mm) was much higher as compared to the mean difference on Day 1 of the intervention (2.16 mm). Even though the gradual increase in mean salivary flow was noted in both groups (Figure 2), there was a significantly greater longitudinal change of salivary flow for the patients in the intervention group, than in the control group (P<0.001) (Table 2).
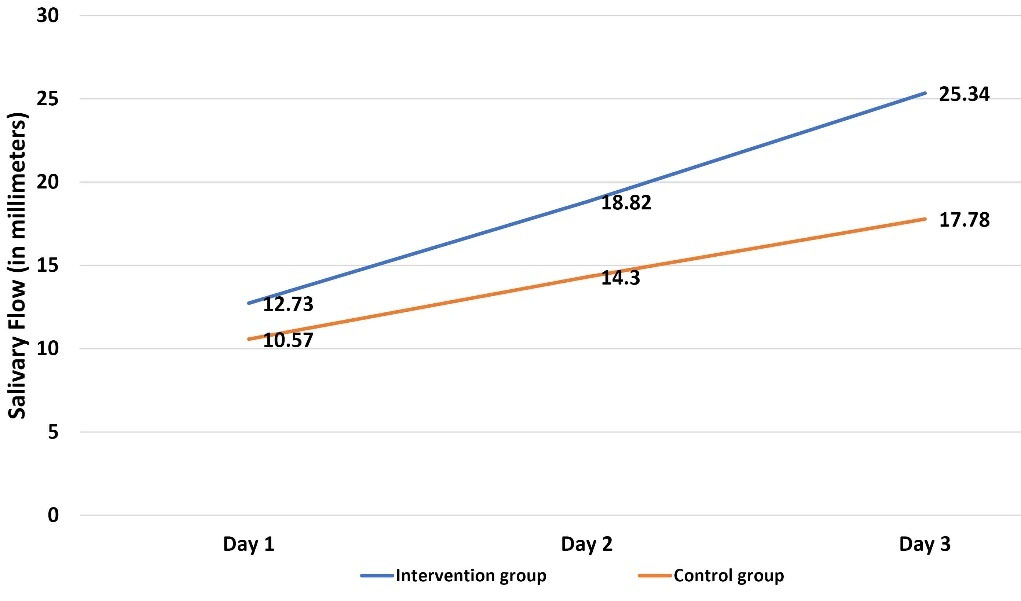
Figure 2.
Comparison of longitudinal change of mean salivary flow between groups
.
Comparison of longitudinal change of mean salivary flow between groups
Table 2.
Comparison of longitudinal change of salivary flow between intervention and control groups (N=92)
|
Time
|
Salivary flow in the intervention group (in mm)
|
Salivary flow in the control group (in mm)
|
P
value
*
|
|
N
|
Mean (SD)
|
N
|
Mean (SD)
|
| Day 1(n=92) |
46 |
12.73(4.93) |
46 |
10.57(3.99) |
<0.001 |
| Day 3(n=92) |
46 |
18.82(4.88) |
46 |
14.30(4.63) |
| Day 7(n=90) |
44 |
25.34(3.94) |
46 |
17.78(5.15) |
*Statistically significant, Repeated Measures Analysis of Variance, P value<0.05.
The comparison of oral intake using the FOIS shows that the median FOIS score in the intervention group was significantly higher than that of the control group from the 3rd day onwards (P<0.001). The time taken to achieve total oral intake (FOIS score of 4-7) for the intervention group was 2 days earlier than that of the control group, with a P value oflt;0.001 (Table 3). Comparison of achievement of total oral intake assessed with FOIS score 4-7 between the groups showed that all the participants in the intervention group achieved total oral intake by the 6th day, whereas all the patients in the control group achieved the same by the 10th day (Figure 3). There is a mild positive correlation between the duration of intubation in hours and the time to resume total oral intake (0.220). Irrespective of the participant’s age, the swallowing, and oral care interventions are effective in achieving total oral intake for the intervention group earlier than the control group (P<0.05 for age<60 and P<0.001 for age>60) (Table 4).
Table 3.
Comparison of oral intake using Functional Oral Intake Scale (FOIS) score between intervention & control group (N=92)
|
Variable
|
Intervention group
|
Control group
|
P
value
*
|
|
N
|
Median (IQR)
|
N
|
Median (IQR)
|
| FOIS score on days after extubation |
| Day 1 (n=92) |
46 |
2.00 (1.0000) |
46 |
2 (1.00) |
0.401 |
| Day 2(n=92) |
46 |
3.00 (0.0000) |
46 |
2.50 (1.00) |
0.013 |
| Day 3 (n=92) |
46 |
4 (1.0000) |
46 |
3 (0.00) |
<0.001 |
| Day 4 (n=92) |
46 |
4 (0.0000) |
46 |
3 (1.00) |
<0.001 |
| Day 5 (n=92) |
46 |
5 (0.0000) |
46 |
4 (1.00) |
<0.001 |
| Day 6 (n=91) |
45 |
5 (0.0000) |
46 |
4 (1.00) |
<0.001 |
| Day 7 (n=90) |
44 |
5 (0.7500) |
46 |
4 (1.00) |
<0.001 |
| Day 8 (n=86) |
42 |
6 (1.0000) |
44 |
5 (1.00) |
<0.001 |
| Day 9 (n=71) |
33 |
6 (0.5000) |
38 |
5 (1.00) |
<0.001 |
| Day 10 (n=43) |
17 |
6 (0.0000) |
26 |
5 (0.25) |
<0.001 |
| Day to achieve total oral intake |
46 |
3 (1.0000) |
46 |
5 (2.00) |
<0.001 |
*Median (interquartile range) and Mann Whitney U test, P value<0.05.
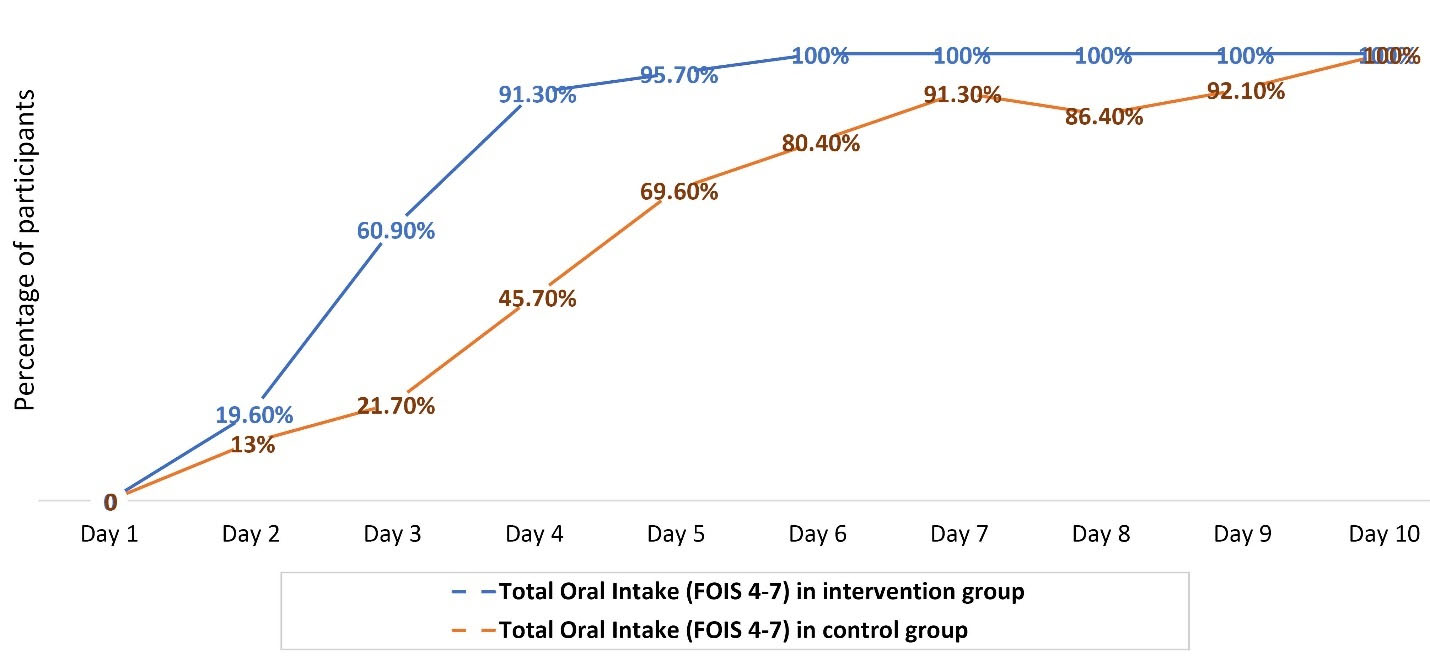
Figure 3.
Comparison of achievement of total oral intake (FOIS score of 4-7) between the groups
.
Comparison of achievement of total oral intake (FOIS score of 4-7) between the groups
Table 4.
Time to resume total oral intake by different age groups N=92
|
Participants
|
Intervention group
|
Control group
|
P
value
*
|
|
N
|
Mean (SD)
(Day to achieve total oral intake)
|
N
|
Mean (SD)
(Day to achieve total oral intake)
|
| Age>60 years |
9 |
3.11 (0.78) |
15 |
6.13 (1.80) |
<0.001 |
| Age≤60 years |
37 |
3.38 (1.03) |
30 |
3.97 (1.32) |
<0.05 |
*Independent student t-test, P value<0.05.
Discussion
Dysphagia is a swallowing disorder that occurs most commonly in patients with neurological or structural impairment of the upper aerodigestive tract. The major etiology behind this is disease conditions like stroke, cancer of the head and neck, or medical procedures like tracheostomy, prolonged intubation, spine surgeries, and mechanical ventilation.1,2,10 Multiple studies are showing increased incidence of dysphagia in post-extubation patients because in these patients neuro-muscular recovery is incomplete and sometimes prolonged.6 Artificial airways can cause airway and laryngeal injuries so that the airway mechanics and protective reflexes will be disrupted. Multiple ventilation cycles can also increase the severity of dysphagia by affecting the synchrony of breathing and swallowing and finally upsetting the nutritional balance of the patients.16 All this evidence points out some effective interventions for post-extubation dysphagia.
A study was conducted regarding the high incidence of dysphagia in post-extubation patients and it revealed an association with adverse outcomes which are clinically relevant. They observed that patients who had post-extubation dysphagia had longer tube feeding, more use of ICU resources like anti-microbial drugs, increased length of hospital stay, and increased intra-hospital 90-day mortality.8 However, some other studies state that the exact frequency of post-extubation dysphagia among all the participants remains unknown due to the absence of a diagnostic standard for dysphagia and small populations represented in existing studies. Specifically, post-extubation dysphagia is associated with a high risk of reintubation, development of pneumonia, longer hospital stay, and reduced dietary intake.9 The swallowing and oral care interventions will be very helpful in resource-poor settings like India as they can reduce the burden of critically ill patients who were extubated but cannot be discharged early due to complications of prolonged intubation.
Total Oral Intake
This study which consisted of SSE, toothbrushing, salivary gland massage, oral cavity, and swallowing exercises revealed that the intervention group had a significant increase in oral intake status according to the FOIS score from 3rd day of the intervention compared to the control group. On daily comparison of the oral intake status between the intervention and control group, the FOIS score for both the groups on the 1st day was in the range of 1-3 (Nil Per Oral, tube feeding). By the 6th day, 100% of the patients in the intervention group achieved a FOIS score of 4-7, and the same was achieved by the control group on the 10th day. These findings were in line with a study by Wu et al which reveals that the participants who got swallowing and oral care interventions were significantly more likely to resume total oral intake (adjusted HR 1.77, 95% CI 1.08 – 2.91), after adjusting for age, intake level, and oxygen supplementation in both the groups. The intervention group in their study took less time to resume total oral intake (14 ± 4.3 days) than the control group (16 ± 2.2 days); moreover, the interventions also kept patients’ oral cavities moist and clean; their lips, tongue, and jaw were moving freely.10 The present study finding was also similar to the previous study by Balou et al where they used exercise-based swallowing intervention in a series of healthy older adults to improve the swallowing function which showed significant improvements in swallowing as represented by improved oral and pharyngeal composite scores of the MBSImP (Modified Barium Swallow Impairment Profile).13
Increased Salivary Flow
The lubricating, anti-microbial, and buffering properties of the saliva have an important role in maintaining a healthy oral cavity.1,2 In patients following prolonged intubation the absence of adequate salivary flow is being observed which can lead to severe xerostomia and contribute to the development of mucositis.17 This study explored the methods to increase the salivary flow in post-extubation patients which helps in the reduction of complications mentioned above. The results showed that swallowing and oral care interventions were significantly effective in increasing the salivary flow in post-extubation patients. The salivary flow was measured on the 1st, 3rd and 7th day of intervention using oral Schirmer’s test, and daily salivary flow was compared between the intervention and control groups. On the 1st day of the intervention, there was only a 2.16 mm difference in the mean salivary flow between the intervention and control group; but, a longitudinal increase in the mean difference of salivary flow between the groups was noted on the 3rd (4.52 mm) and 7th day (7.56 mm). A previous study revealed similar results where effects of salivary gland massage in alleviating the symptoms of dry mouth in elderly nursing home residents. It showed that there was a significant increase in water concentration on the cheek mucous membrane after 2 weeks course of massage twice daily(P < 0.05).11 Another interesting finding was from a study conducted by Affoo et al to determine whether manual (MTB) or electric toothbrushing (ETB) modulates the whole salivary flow rate in older adults. It revealed that a significant, increase in salivary flow was during MTB and ETB but the effect sizes associated with salivary flow rate were similar (MTB: P < 0.004, ETB: P < 0.005).18
Relationship Between Oral Intake and Baseline Variables
Previous studies have shown that prolonged mechanical ventilation was significantly associated with severe cases of post-extubation dysphagia19-21which compromises the oral intake of the patient. However, the current study shows that the duration of intubation only had a mild positive correlation with total oral intake (-0.220). A study by Tsai et al revealed that high rates of post-extubation swallowing dysfunction were present in participants aged 65 years and older. Since recovery for these participants was not spontaneous, they were recommending the development of effective swallowing interventions.4,22,23 Present study shows that swallowing and oral care interventions were effective for all the participants in the intervention group irrespective of their age group. Contrary to this finding, a study conducted by Wu et al shows that older participants (at least 65 years) who received swallowing and oral care interventions were 2.47-fold more likely to resume total oral intake than the younger participants (50 -64 years).10,24
Although the interventions in this study had demonstrated significant effects in resuming early oral intake and increased salivary flow in patients following endotracheal extubation, it had some limitations. Firstly, there were no instrumental or radiographical methods used for confirming the underlying reasons for dysphagia, and extent of impairments in each individual; and how these swallowing and oral care interventions were helping the individuals to attain early oral intake by improving the swallowing physiology. Secondly, the sample size and period of the study were not sufficient to assess various factors associated with the development of post-extubation which was very important in the development of prevention strategies. Thirdly, this study consisted of multiple interventions, making it difficult to identify which intervention was most effective. These limitations can reduce the generalizability of the study.
Conclusion
There are drastic advances in the field of critical care nowadays, however a genuine solution for post-extubation dysphagia in critically ill patients is a challenge for health professionals. Nurse-led swallowing and oral care interventions already have proven themselves to improve the oral intake and salivary flow in post-extubation patients and thereby aid in a better quality of life. It also helps with the judicious use of ICU resources as it helps in the early discharge of the patient. On par with the already existing literature that supports the swallowing and oral care interventions, the current study has also proved that this intervention is effective in increasing oral intake and salivary flow and thereby controlling some of the complications associated with prolonged intubation. The swallowing and oral care interventions have been adopted by various hospitals around the world due to their effectiveness and it is high time to adopt the same in our health settings too.
Acknowledgments
The authors would like to acknowledge the Nursing staff of the Intensive care units and wards, where the study is conducted for the support rendered in conducting the study.
COI-statement
The authors declared no conflict of interest in this study.
Data Availability Statement
The datasets are available from the corresponding author upon reasonable request.
Ethical Approval
Permission was obtained for the current study from Institute Nursing Research Monitoring Committee (CON/NRMC/M.Sc./2020/MSN/6) and the Institute Ethics Committee for Human Studies (CON/IEC/M. Sc/2020/MSN/6). The study was registered under the Clinical Trial Registry India (CTRI/2021/12/038773). The procedures followed were by the ethical standards of the institution as well as the Declaration of Helsinki revised in 2013. After a brief explanation to each participant regarding the study, informed consent was obtained from them. Data confidentiality, the anonymity of the subjects, and the right to withdraw from the study were explained to participants before data collection.
Research Highlights
What is the current knowledge?
-
Swallowing and oral care interventions, along with standard oral care, are an essential part of rehabilitation strategies following endotracheal extubation, which can reduce the development of complications associated with prolonged intubation.
What is new here?
-
Nurse-led swallowing and oral care interventions were effective in improving oral intake and salivary flow in post-extubation patients, thereby aiding in improving the nutritional status and a better quality of life.
-
It also helps with the judicious use of ICU resources as it helps the early discharge of the patient.
References
- Chen CC, Wu KH, Ku SC, Chan DC, Lee JJ, Wang TG. Bedside screen for oral cavity structure, salivary flow, and vocal production over the 14 days following endotracheal extubation. J Crit Care 2018; 45:1-6. doi: 10.1016/j.jcrc.2017.11.035 [Crossref] [ Google Scholar]
- Klahn MS, Perlman AL. Temporal and durational patterns associating respiration and swallowing. Dysphagia 1999; 14(3):131-8. doi: 10.1007/pl00009594 [Crossref] [ Google Scholar]
- Martin-Harris B, Brodsky MB, Price CC, Michel Y, Walters B. Temporal coordination of pharyngeal and laryngeal dynamics with breathing during swallowing: single liquid swallows. J Appl Physiol (1985) 2003; 94(5):1735-43. doi: 10.1152/japplphysiol.00806.2002 [Crossref] [ Google Scholar]
- Tsai MH, Ku SC, Wang TG, Hsiao TY, Lee JJ, Chan DC. Swallowing dysfunction following endotracheal intubation: age matters. Medicine (Baltimore) 2016; 95(24):e3871. doi: 10.1097/md.0000000000003871 [Crossref] [ Google Scholar]
- El Solh A, Okada M, Bhat A, Pietrantoni C. Swallowing disorders post orotracheal intubation in the elderly. Intensive Care Med 2003; 29(9):1451-5. doi: 10.1007/s00134-003-1870-4 [Crossref] [ Google Scholar]
- Ponfick M, Linden R, Nowak DA. Dysphagia--a common, transient symptom in critical illness polyneuropathy: a fiberoptic endoscopic evaluation of swallowing study. Crit Care Med 2015; 43(2):365-72. doi: 10.1097/ccm.0000000000000705 [Crossref] [ Google Scholar]
- Kim MJ, Park YH, Park YS, Song YH. Associations between prolonged intubation and developing post-extubation dysphagia and aspiration pneumonia in non-neurologic critically ill patients. Ann Rehabil Med 2015; 39(5):763-71. doi: 10.5535/arm.2015.39.5.763 [Crossref] [ Google Scholar]
- Schefold JC, Berger D, Zürcher P, Lensch M, Perren A, Jakob SM. Dysphagia in mechanically ventilated ICU patients (DYnAMICS): a prospective observational trial. Crit Care Med 2017; 45(12):2061-9. doi: 10.1097/ccm.0000000000002765 [Crossref] [ Google Scholar]
- Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care 2011; 15(5):R231. doi: 10.1186/cc10472 [Crossref] [ Google Scholar]
- Wu CP, Xu YJ, Wang TG, Ku SC, Chan DC, Lee JJ. Effects of a swallowing and oral care intervention for patients following endotracheal extubation: a pre- and post-intervention study. Crit Care 2019; 23(1):350. doi: 10.1186/s13054-019-2623-2 [Crossref] [ Google Scholar]
- López-Jornet P, Camacho-Alonso F, Bermejo-Fenoll A. A simple test for salivary gland hypofunction using Oral Schirmer’s test. J Oral Pathol Med 2006; 35(4):244-8. doi: 10.1111/j.1600-0714.2006.00411.x [Crossref] [ Google Scholar]
- Ono K, Uchiyama K. Evaluation of a new salivary gland massage with oil for elderly nursing home residents. Int J Phys Ther Rehabil 2017; 3:129. doi: 10.15344/2455-7498/2017/129 [Crossref] [ Google Scholar]
- Byeon H. Effect of orofacial myofunctional exercise on the improvement of dysphagia patients’ orofacial muscle strength and diadochokinetic rate. J Phys Ther Sci 2016; 28(9):2611-4. doi: 10.1589/jpts.28.2611 [Crossref] [ Google Scholar]
- Balou M, Herzberg EG, Kamelhar D, Molfenter SM. An intensive swallowing exercise protocol for improving swallowing physiology in older adults with radiographically confirmed dysphagia. Clin Interv Aging 2019; 14:283-8. doi: 10.2147/cia.s194723 [Crossref] [ Google Scholar]
- Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005; 86(8):1516-20. doi: 10.1016/j.apmr.2004.11.049 [Crossref] [ Google Scholar]
- Zuercher P, Moret CS, Dziewas R, Schefold JC. Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Crit Care 2019; 23(1):103. doi: 10.1186/s13054-019-2400-2 [Crossref] [ Google Scholar]
- Dennesen P, van der Ven A, Vlasveld M, Lokker L, Ramsay G, Kessels A. Inadequate salivary flow and poor oral mucosal status in intubated intensive care unit patients. Crit Care Med 2003; 31(3):781-6. doi: 10.1097/01.ccm.0000053646.04085.29 [Crossref] [ Google Scholar]
- Affoo RH, Trottier K, Garrick R, Mascarenhas T, Jang Y, Martin RE. The effects of tooth brushing on whole salivary flow rate in older adults. Biomed Res Int 2018; 2018:3904139. doi: 10.1155/2018/3904139 [Crossref] [ Google Scholar]
- Hongo T, Yamamoto R, Liu K, Yaguchi T, Dote H, Saito R. Association between timing of speech and language therapy initiation and outcomes among post-extubation dysphagia patients: a multicenter retrospective cohort study. Crit Care 2022; 26(1):98. doi: 10.1186/s13054-022-03974-6 [Crossref] [ Google Scholar]
- Brodsky MB, Pandian V, Needham DM. Post-extubation dysphagia: a problem needing multidisciplinary efforts. Intensive Care Med 2020; 46(1):93-6. doi: 10.1007/s00134-019-05865-x [Crossref] [ Google Scholar]
- El Gharib AZG, Berretin-Felix G, Rossoni DF, Seiji Yamada S. Effectiveness of therapy on post-extubation dysphagia: clinical and electromyographic findings. Clin Med Insights Ear Nose Throat 2019; 12:1179550619873364. doi: 10.1177/1179550619873364 [Crossref] [ Google Scholar]
- Xia C, Ji J. The characteristics and predicators of post-extubation dysphagia in ICU patients with endotracheal intubation. Dysphagia 2023; 38(1):253-9. doi: 10.1007/s00455-022-10462-0 [Crossref] [ Google Scholar]
- Hara K, Tohara H, Minakuchi S. Treatment and evaluation of dysphagia rehabilitation especially on suprahyoid muscles as jaw-opening muscles. Jpn Dent Sci Rev 2018; 54(4):151-9. doi: 10.1016/j.jdsr.2018.06.003 [Crossref] [ Google Scholar]
- Christensen M, Trapl M. Development of a modified swallowing screening tool to manage post-extubation dysphagia. Nurs Crit Care 2018; 23(2):102-7. doi: 10.1111/nicc.12333 [Crossref] [ Google Scholar]