Journal of Caring Sciences. 13(2):97-105.
doi: 10.34172/jcs.33331
Original Article
An Examination of the Agreement between Self-reported Diabetes and Paraclinical Tests, Medical Records, and Clinical Examinations: Insights from the Shahedieh Cohort Study, Yazd, Iran
Farzan Madadizadeh Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing, 
Mahdieh Momayyezi Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, * 
Hossein Fallahzadeh Conceptualization, Investigation, Validation, Writing – review & editing, 
Author information:
Departments of Biostatistics and Epidemiology, Center for Healthcare Data Modeling, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Abstract
Introduction:
Many researchers utilize self-reports to evaluate the prevalence of diseases. However, the accuracy of these self-reports remains uncertain in various studies. The objective of this particular study was to validate self-reported cases of diabetes among adults aged 35-70 years participating in the Shahedieh Cohort Study (SHCS).
Methods:
This cross-sectional study was conducted using data from the first phase of SHCS during 2015-2017. The study included 1000 Iranian adults aged 35-70 years. The Gold standard for diabetes was determined by measuring fasting blood sugar (FBS) and evaluating the history of treatment and use of diabetes medications. To assess self-report validity, various statistical indices such as sensitivity, specificity, positive and negative predictive values (NPVs), accuracy, positive likelihood ratio (LR+), negative likelihood ratio (LR-) and AUC were used. The agreement between self-reported diabetes and the gold standard was assessed using kappa statistics. All statistical analyses were performed using SPSS version 13 and R 4.3.1 software.
Results:
The study findings indicated that the prevalence of diabetes was 18% according to self-report and 19.9% according to the gold standard measurement. The self-report accuracy was 95.67%. There was perfect agreement (kappa=0.86) between the self-report and gold standard criteria. The AUC, sensitivity and specificity of self-reported diabetes were 0.937, 93.82% and 96.08%, respectively. Additionally, the results suggested that the self-report of diabetes was more valid in individuals with a normal body mass index (BMI) and without a family history of diabetes in first-degree relatives.
Conclusion:
The results showed that in the absence of diabetes control programs, self-report of diabetes is reliable and recommended.
Keywords: Agreement, Self-report, Clinical examination, Diabetes
Copyright and License Information
© 2024 The Author(s).
This work is published by Journal of Caring Sciences as an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (
http://creativecommons.org/licenses/by-nc/4.0/). Non-commercial uses of the work are permitted, provided the original work is properly cited.
Funding Statement
Shahid Sadoughi University of Medical Sciences (Project No: 8991).
Introduction
Diabetes is one of the most common non-communicable diseases in Iran. There are common ways to diagnose diabetes. The most common way to diagnose this disease is to measure fasting blood sugar (FBS). Atlas of STEPwise approach to non-communicable disease (NCD) risk factor surveillance (STEPs) 2021 showed that the prevalence of type 2 diabetes based on FBS (FBS ≥ 126) in Yazd province was 18.06%, which was higher than the national prevalence (14.15%). Based on the FBS index, Yazd province was fourth in terms of diabetes in Iran. Also, the prevalence of diabetes based on glycated hemoglobin (HbA1c) (≥ 6.5) in Yazd province was 23.8%, which was higher than the national prevalence (17.52%). Based on the HBA1c index, Yazd province was ranked first in Iran in terms of diabetes.1
It is also important that many people do not know that they have diabetes. It means that a person may not be aware of having diabetes, while the complications of the diseases are spreading in his body. The results of the STEPs study in 2021 showed that the awareness percentage of diabetes in Yazd province was 81.55%, which was higher than the national rate (73.29%). Based on this index, Yazd province ranked eighth among the 31 provinces of Iran. Also, the level of awareness of diabetes in men was higher than women.1
The evaluation of data collection tools (questionnaires, interviews, examinations, medical tests, and self-report) to obtain an accurate prevalence of the disease at the community level is essential. One of the appropriate and advantageous methods for collecting information on chronic diseases is self-reporting. Self-reporting is a quick and easy method to assess disease prevalence. On the other hand, it leads to saving time and money.2 According to people’s awareness of diseases in different regions, individual self-report can be used to assess the chronic diseases prevalence. The results of prevalence studies based on self-report should be expounded with wariness. Also, the validity of self-report in these studies should be checked.3
The use of the self-report method by researchers to obtain appropriate data is increasing. On the other hand, if the prevalence of the disease is determined based on self-report, the validity of self-report data should be confirmed.4 Self-reported diabetes is a usual approach of determining diabetes in large populations in epidemiological studies. It seems that self-reported diabetes is used as an appropriate way to assess the prevalence of type 2 diabetes in various countries such as Brazil, Japan, America, and Spain.5 The accuracy of the obtained data can be influenced by age, education, gender, medical information, and the number of visits to the doctor. Disagreement between the self-report of diabetes and the GOLD criteria can lead to distortion in the results of prevalence studies.5
The importance of examining the agreement between self-reported diabetes, paraclinical tests, medical records, and clinical examinations lies in the fact that diabetes is a chronic and complex disease that requires accurate diagnosis and management. Self-reported diabetes is often used as a screening tool in epidemiological studies due to its convenience, but it may not always accurately reflect the true prevalence or incidence of diabetes. Paraclinical tests, such as fasting blood glucose and HbA1c, are commonly used to diagnose diabetes, but their accuracy may be affected by factors such as fasting status and glycemic variability. Medical records and clinical examinations provide additional information about diabetes diagnosis and management but may be subjective or incomplete due to errors in documentation or recall bias. Therefore, it is essential to examine the agreement between these sources of information to improve diabetes diagnosis, management, and research by identifying areas of agreement and disagreement, understanding the factors that influence agreement, and developing strategies to improve accuracy and consistency in diabetes diagnosis and management.
Recently, the Persian Cohort Study was conducted to determine the effective factors in causing common non-communicable diseases in Iran with the participation of different universities in Iran. This study was conducted in Yazd province under the title of the Shahedieh Cohort Study (SHCS). Since cohort studies will be the basis for many articles, the accuracy of self-reporting of the disease should be confirmed. Considering that no study has determined the validity of self-report of diabetes in the SHCS, this study aimed to investigate the agreement between self-reported diabetes and Para clinical tests, medical records, and clinical examinations.
Material and Methods
This study is an analytical cross-sectional study. This study was performed on the data of the first phase of the SHCS in Yazd during 2015-2017. The SHCS was conducted to assess non-communicable diseases and their risk factors in 1000 Iranian population adults aged 35-70 years from Shahedieh, Zarch, and Ashekzar cities in Yazd province.6
The SHCS is a study based on population that is part of the Persian prospective cohort study. The Persian prospective cohort study was conducted in 18 area of Iran.7 In the Persian prospective cohort study, many variables included: demographic-social characteristics, history of chronic diseases, medication use and smoking, sleep status, personal habits (nutrition, physical activity), and anthropometric indices were completed through questionnaires, examinations, and biochemical tests.
The SHCS involved four stages of data collection. Initially, individuals were invited to participate and visited the study center to be assigned a unique code (IRCT) and registered for future visits after providing consent. Appointments were then scheduled for subsequent data collection stages. In the next step, a blood test was taken from the person at the scheduled appointment. Sampling was measured after 12 hours of fasting through a blood test (25 mL). The test results were entered into the software after preparation by the laboratory technician. After blood sampling, individuals’ anthropometric measurements such as height, weight, and waist circumference were taken in a fasting state by a trained person using standard methods. These measurements were recorded simultaneously in the software. Following the measurements, the questionnaire’s queries were put forward to individuals in three different categories (general, medical, and nutrition section) by trained personnel through face-to-face interviews. Each section of the questionnaire (general questions, medical questions, nutrition questions) was asked by a separate person while responses were simultaneously recorded in software.
Based on the provided information about the timing of the blood tests, questionnaire completion, and availability of test results, it is highly unlikely that performing the FBS test would affect people’s self-reported diabetes. The blood tests and questionnaire were completed on the same day, but the test results were not immediately available. This means that individuals were not aware of their FBS test results at the time they completed the self-report questionnaire regarding their diabetes status. Therefore, it is reasonable to assume that the FBS test results did not influence their self-reported diabetes status during the study period.
In the present study, to determine self-reported diabetes, people were asked: “Do you have a history of diabetes?” (Yes/No). The GOLD criteria for diagnosis of Type 2 diabetes is defined as FBS ≥ 126 mg/dL and/or positive history of relevant medicine use (insulin, glibenclamide, metformin, gliclazide) and Positive history of diabetes treatment.
FBS was measured after 12 hours of fasting through a blood test (25 mL). After transferring the samples to the laboratory, biochemical analysis was performed using BT-1500 Autoanalyzer (BT-1500, Biotecnica, Italy).6 Other variables used included demographic variables (age, gender, height, weight, marital status, education level), self-reported diabetes (Having diabetes, history of diabetes treatment, family history of diabetes, medications history), smoking, drug use and alcohol use were used. The medication history was obtained by separately asking the list of all drugs mentioned in the Persian Cohort protocol from the participants.
Based on self-report, people were divided into two groups (diabetic patients and healthy people), and their self-report was compared with the GOLD criteria. Then, false positives (FP) (According to self-report, they had diabetes but were healthy according to the GOLD criteria), true positive (TP) (According to self-report, they had diabetes and also had diabetes according to the GOLD criteria), false negative (FN) (According to self-report, they were healthy but had diabetes according to the GOLD criteria), and true negative (TN) (According to self-report and GOLD criteria, they were healthy).
To assess the validity of the self-report, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive (LR + ) and negative likelihood ratio (LR-), agreement rate, and kappa coefficient were calculated in R software and using the bootLR package. The ability of a test to find cases of disease is called sensitivity. To calculate the sensitivity of a test, the proportion of true positives must be divided by the total of true positives and false negatives. The ability of a test to find people without the disease is called specificity. To calculate the specificity of a test, the proportion of true negative cases should be divided by the total of true negative and false positive cases. To calculate the LR + , the proportion of patients who have a positive test is divided by the proportion of healthy people who have a positive test (LR + = sensitivity/1- specificity). To calculate the LR-, the proportion of healthy people who have a positive test is divided by the proportion of patients who have a negative test (LR- = 1- sensitivity/ specificity).
The factors related to the agreement between self-reporting and the GOLD criteria, as well as FP (over-reporting) and FN (under-reporting), investigate with the univariate and multivariate logistic regression in SPSS version 20 software. At first, variables were examined separately in the univariate regression. Then, the multivariate regression method was used to determine predictors. To evaluate the agreement between self-report and the GOLD criteria, Fleiss’ kappa statistic was calculated. Based on kappa statistics, the agreement was classified as follows: slight agreement (0-0.20); fair agreement (0.21–0.40); moderate agreement (0.41–0.60); substantial agreement (0.61–0.80); and almost perfect agreement (0.81–1.00).8The Fleiss’ kappa statistic, which takes into account chance agreement, is defined as (observed agreement−expected agreement)/(1−expected agreement). The FBS test was not available for 107 individuals, who were considered as missing data.
The receiver operating characteristic curve (ROC) is used to identify performance of self-reporting in diabetes recognition. The present study has ethics approval from the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, and Code: IR.SSU.SPH.REC.1399.238. Also, the principles related to the voluntary nature of the study and the confidentiality of their information has been observed. The SHCS was carried out following the principles outlined in the Declaration of Helsinki, and either the participants or representatives of those who were illiterate provided informed consent.
Results
According to the results 18% of people had diabetes based on self-report and 19.9% based on the GOLD criteria. Table 1 showed that 14.7% had FBS higher than 126 mg/dL, and 15.6% had a history of diabetes treatment. Also, FBS was not controlled in 65.1% of people who had a history of diabetes treatment. The findings showed that 26.4% of diabetic people (based on the GOLD criteria) had a family history of diabetes in their first-degree relatives. According to the results, 15.9 % of patients who had diabetes based on the Golden Standard were unaware that they had diabetes. Also, among people who reported they had diabetes, 1.4% did not have confirmed diabetes (Table 2).
Table 1.
Characteristics related to diabetes in participants of the Shahedieh Cohort Study (n = 9515)
|
Variable
|
No. (%)
|
| Self-reported diabetes |
|
| No |
7802 (82) |
| Yes |
1713 (18) |
| Total |
9515 (100) |
| GOLD criteria diabetes |
|
| No |
7510 (79.8) |
| Yes |
1898 (20.2) |
| Total |
9408 (100) |
| Family history of diabetes |
|
| No |
3999 (42.1) |
| Yes |
5495 (57.9) |
| Total |
9494 (100) |
| Being treated for diabetes |
|
| No |
8034 (84.4) |
| Yes |
1480 (15.6) |
| Total |
9514 (100) |
| Fasting blood sugar |
|
| < 126 |
8025 (85.3) |
| ≥ 126 |
1384 (14.7) |
| Total |
9408 (100) |
Table 2.
Validity of self-reported diabetes in participants of the Shahedieh Cohort Study
|
Self-reported diabetes
|
GOLD criteria,
No. (%)
|
Accuracy
|
Kappa
|
Sensitivity
|
Specificity
|
LR+
|
LR-
|
PPV
|
NPV
|
AUC
|
|
Yes
|
No
|
| Yes |
1596 (84.1) |
105 (1.4) |
95.67 (95.24-96.08) |
86 (84.2-88.2) |
93.82 (92.58-94.92) |
96.08 (95.62-96.5) |
23.93 (21.42-26.76) |
0.06 (0.05-0.08) |
84.09 (82.54-85.52) |
98.6 (98.32-98.84) |
0.937 |
| No |
302 (15.9) |
7405 (98.6) |
According to Table 2, the accuracy of self-reported diabetes was 95.67%. Also, perfect agreement was obtained between self-reported diabetes and the GOLD criteria (kappa = 0.86, CI = 84.2-88.2). The sensitivity, specificity, PPV, NPV, LR + , and LR- are shown in Table 2. According to the results, the self-reported ability to find disease cases was 93.82%, and the self-reported ability to find healthy people was 96.08%, that were high percentage. The results also showed that the GOLD criteria result was consistent with the positive self-reported in 84% of cases (It is a positive self-report, and the disease has been confirmed according to the GOLD criteria). The GOLD criteria result was consistent with the negative self-reported in 98% of the participants (It is a negative self-report and the people is healthy according to the golden standard).
The multivariate logistic regression after adjusting for confounders showed that body mass index (BMI) and family history of diabetes were associated with disagreement between self-report and the GOLD criteria. The odds of disagreement in people with a family history of diabetes was 45% higher than other people (OR = 1.45, P = 0.001). According to Table 3, the odds of disagreement was 31% less in overweight people (OR = 0.69, P =0.001) and 65% less in people with normal BMI than obese people (OR = 0.35, P < 0.001).
Table 3.
Logistic regression of the factors affecting disagreement between self-reported diabetes and the GOLD criteria in the Shahideh Cohort Study
|
Determinants (diabetes)
|
Discordance, No. (%)
|
Discordance (95% CI)
|
|
Crude OR
|
P
value
a
|
Adjusted OR
|
P
value
b
|
| Gender |
|
|
|
|
|
| Female |
212/4712 (4.5) |
1 (reference) |
- |
- |
- |
| Male |
195/4696 (4.2) |
1.08 (0.89-1.32) |
0.401* |
- |
- |
| Age |
|
|
|
|
|
| 35-45 |
154/3822 (4) |
1 (reference) |
- |
1 (reference) |
- |
| 45-55 |
125/2940 (4.3) |
1.05 (0.83-1.34) |
0.641* |
1.03 (0.81-1.32) |
0.771* |
| 55-65 |
100/2044 (4.9) |
1.22 (0.94-1.58) |
0.122* |
1.24 (0.95-1.6) |
0.105* |
| > 65 |
28/602 (4.7) |
1.16 (0.76-1.75) |
0.470* |
1.17 (0.77-1.78) |
0.432* |
| BMI |
|
|
|
|
|
| Less than 18.5 |
0 |
0 |
- |
- |
- |
| 18.5 to < 25 |
44/2060 (2.1) |
0.34 (0.34-1.24) |
< 0.001* |
0.35 (0.25-0.49) |
< 0.001* |
| 25 to < 30 |
165/3933 (4/2) |
0.68 (0.68-1.55) |
< 0.001* |
0.69 (0.56-0.86) |
0.001* |
| 30 or higher |
191/3173 (6) |
1 (reference) |
- |
- |
- |
| Marital status |
|
|
|
|
|
| Married |
388/9003 (4.3) |
1 (reference) |
- |
- |
- |
| Single |
19/405 (4.7) |
091 (0.57-1.46) |
0.702* |
- |
- |
| Education |
|
|
|
|
|
| Illiterate |
72/1559 (4.6) |
1 (reference) |
- |
- |
- |
| Elementary school |
122/2932 (4.2) |
0.89 (0.66-1.2) |
0.470* |
- |
- |
| Middle school |
66/1561 (4.2) |
0.91 (0.64-1.28) |
0.590* |
- |
- |
| Diploma |
83/1899 (4.4) |
0.94 (0.68-1.3) |
0.723* |
- |
- |
| University education |
64/1451 (4.4) |
0.95 (0.67-1.34) |
0.781* |
- |
- |
| Smoking status |
|
|
|
|
|
| No |
343/8058 (4.3) |
1 (reference) |
- |
- |
- |
| Yes |
64/1350 (4.7) |
1.11 (0.85-1.47) |
0.412* |
- |
- |
| Family history of diabetes |
|
|
|
|
|
| No |
132/3946 (3.3) |
1 (reference) |
- |
1 (reference) |
- |
| Yes |
275/5441 (5.1) |
1.53 (1.24-1.9) |
< 0.001* |
1.45 (1.17-1.8) |
0.001* |
| Drugs use |
|
|
|
|
|
| No |
342/7858 (4.4) |
1 (reference) |
- |
- |
- |
| Yes |
65/1550 (4.2) |
0.96 (0.73-1.26) |
0.771* |
- |
- |
| Alcohol use |
|
|
|
|
| No |
375/8611 (4.4) |
1 (reference) |
- |
- |
- |
| Yes |
32/796 (4) |
0.92 (0.63-1.33) |
0.651* |
- |
- |
a Univariate; b Multivariate logistic regression; *Statistically significant.
The multivariate logistic regression showed that the odds of FP (over-reporting) in people with a family history of diabetes was 75% higher than other people (OR = 1.75, P = 015). Also, the odds of over-reporting diabetes was 58% lower in people with normal BMI (OR = 0.42, P = 0.009) and 36% lower in overweight people than obese people (OR = 0.64, P = 0.04) (Table 4).
Table 4.
Logistic regression of the factors affecting over-reporting of diabetes (false positive) in the Shahideh Cohort Study
|
Determinants
|
Discordance,
No. (%)
|
False positive (95% CI)
|
|
Crude OR
|
P
value
a
|
Adjusted OR
|
P
value
b
|
| Gender |
|
|
|
|
|
| Female |
72/4712 (1.5) |
1 (reference) |
- |
1 (reference) |
- |
| Male |
33/4697 (0.7) |
2.19 (1.45-3.31) |
< 0.001* |
1.76 (1.09-2.82) |
0.195* |
| Age |
|
|
|
|
|
| 35-45 |
42/3823 (1.1) |
1 (reference) |
- |
- |
- |
| 45-55 |
34/2940 (1.2) |
1.05 (0.66-1.66) |
0.822* |
- |
- |
| 55-65 |
23/2044 (1.1) |
1.02 (0.61-1.7) |
0.921* |
- |
- |
| > 65 |
6/696 (0.9) |
0.78 (0.33-1.84) |
0.570* |
- |
- |
| BMI |
|
|
|
|
|
| Less than 18.5 |
0 |
0 |
- |
0 |
- |
| 18.5 to < 25 |
12/2060 (0.6) |
0.33 (0.18-0.63) |
0.001* |
0.42 (0.22-0.8) |
0.009* |
| 25 to < 30 |
38/3934 (1) |
0.56 (0.36-0.85) |
0.007* |
0.64 (0.42-0.98) |
0.042* |
| 30 or higher |
54/3173 (1.7) |
1 (reference) |
- |
1 (reference) |
- |
| Marital status |
|
|
|
|
|
| Married |
102/9089 (1.1) |
1 (reference) |
- |
- |
- |
| Single |
3/414 (0.7) |
1.55 (0.49-4.92) |
0.451* |
- |
|
| Education |
|
|
|
|
|
| Illiterate |
16/1571 (1) |
1 (reference) |
- |
- |
- |
| Elementary school |
28/2960 (0.9) |
0.92 (0.5-1.72) |
0.812* |
- |
- |
| middle school |
17/1575 (1.1) |
1.06 (0.53-2.1) |
0.865* |
- |
- |
| Diploma |
24/1920 (1.3) |
1.23 (0.65-2.32) |
0.524* |
- |
- |
| University education |
20/1467 (1.4) |
1.34 (0.69-2.6) |
0.380* |
- |
- |
| Smoking status |
|
|
|
|
|
| No |
96/8059 (1.2) |
1 (reference) |
- |
1 (reference) |
- |
| Yes |
9/1350 (0.7) |
0.55 (0.28-1.1) |
0.090* |
0.95 (0.44-2.04) |
0.901* |
| Family history of diabetes |
|
|
|
|
|
| No |
29/3995 (0.7) |
1 (reference) |
- |
1 (reference) |
- |
| Yes |
76/5487 (1.4) |
1.92 (1.25-2.95) |
0.003* |
1.71 (1.11-2.64) |
0.015* |
| Drugs use |
|
|
|
|
|
| No |
88/7858 (1.1) |
1 (reference) |
- |
- |
- |
| Yes |
17/1551 (1.1) |
1.02 (0.6-1.72) |
0.936* |
- |
- |
| Alcohol use |
|
|
|
|
|
| No |
97/8612 (1.1) |
1 (reference) |
- |
- |
- |
| Yes |
8/796 (1) |
0.89 (0.43-1.83) |
0.754* |
- |
- |
aUnivariate; bMultivariate logistic regression; *Statistically significant.
Table 5 showed that increasing BMI, smoking, and having a family history of diabetes in first-degree relatives increased the odds of FP (under-reporting). So, the odds of under-reporting diabetes in smokers was 36% higher than non-smokers (OR = 1.36, P = 0.034). This odds for people with a history of diabetes in first-degree relatives was 43% higher than other people (OR = 1.43, P = 0.014). Also, the results indicated that the odds of under-reporting diabetes was 30% less in overweight people (OR = 0.7, P = 0.006) and 68% less in people with normal BMI than obese people (OR = 0.32, P < 0.001). The study found that individuals’ self-reported performance in accurately diagnosing diabetes had high sensitivity (93.82%) and specificity (96.08%), as well as a high area under ROC curve (0.937) (Figure 1).
Table 5.
Logistic regression of the factors affecting under-reporting of diabetes (false negative) in the Shahideh cohort study
|
Determinants
|
Discordance,
No. (%)
|
False negative (95% CI)
|
|
Crude OR
|
P
value
a
|
Adjusted OR
|
P
value
b
|
| Gender |
|
|
|
|
|
| Female |
140/4712 (3) |
1 (reference) |
- |
1 (reference) |
- |
| Male |
162/4697 (3.4) |
0.85 (0.68-1.07) |
0.180* |
0.8 (0.61-1.04) |
0.092* |
| Age |
|
|
|
|
|
| 35-45 |
112/3822 (2.9) |
1 (reference) |
- |
1 (reference) |
- |
| 45-55 |
91/2940 (3.1) |
1.05 (0.79-1.4) |
0.691* |
1.05 (0.79-1.4) |
0.703* |
| 55-65 |
77/2045 (3.8) |
1.29 (0.96-1.74) |
0.083* |
1.31 (0.97-1.77) |
0.071* |
| > 65 |
22/613 (3.6) |
1.23 (0.77-1.96) |
0.371* |
1.28 (0.806-2.05) |
0.283* |
| BMI |
|
|
|
|
|
| Less than 18.5 |
0 |
0 |
- |
- |
- |
| 18.5 to < 25 |
32/2060 (1.6) |
0.35 (0.23-0.51) |
< 0.001* |
0.32 (0.21-0.47) |
< 0.001* |
| 25 to < 30 |
127/3934 (3.2) |
0.73 (0.57-0.94) |
0.016* |
0.7 (0.54-0.9) |
0.006* |
| 30 or higher |
137/3173 (4.3) |
1 (reference) |
- |
1 (reference) |
- |
| Marital status |
|
|
|
|
|
| Married |
286/9013 (3.2) |
1 (reference) |
- |
- |
- |
| Single |
16/407 (3.9) |
0.8 (0.47-1.33) |
0.391* |
- |
- |
| Education |
|
|
|
|
|
| Illiterate |
56/1559 (3.6) |
1 (reference) |
- |
- |
- |
| Elementary school |
94/2934 (3.2) |
1.19 (0.79-1.78) |
0.390* |
- |
- |
| middle school |
49/1565 (3.1) |
1.05 (0.73-1.52) |
0.754* |
- |
- |
| Diploma |
59/1903 (3.1) |
1.03 (0.68-1.56) |
0.873* |
- |
- |
| University education |
44/1452 (3) |
1.02 (0.68-1.52) |
0.901* |
- |
- |
| Smoking status |
|
|
|
|
|
| No |
247/8059 (3.1) |
1 (reference) |
- |
1 (reference) |
- |
| Yes |
55/1350 (4.1) |
1.34 (0.99-1.81) |
0.050* |
1.43 (1.02-2) |
0.034* |
| Family history of diabetes |
|
|
|
|
|
| No |
103/3950 (2.6) |
1 (reference) |
- |
1 (reference) |
- |
| Yes |
199/5449 (3.7) |
1.41 (1.11-1.8) |
0.005* |
1.36 (1.06-1.74) |
0.014* |
| Drugs use |
|
|
|
|
|
| No |
254/7859 (3.2) |
1 (reference) |
- |
- |
- |
| Yes |
48/1550 (3.1) |
0.95 (0.69-1.3) |
0.781* |
- |
- |
| Alcohol use |
|
|
|
|
|
| No |
278/8612 (3.2) |
1 (reference) |
- |
- |
- |
| Yes |
24/796 (3) |
0.93 (0.61-1.42) |
0.745* |
- |
- |
aUnivariate; bMultivariate logistic regression; *Statistically significant.
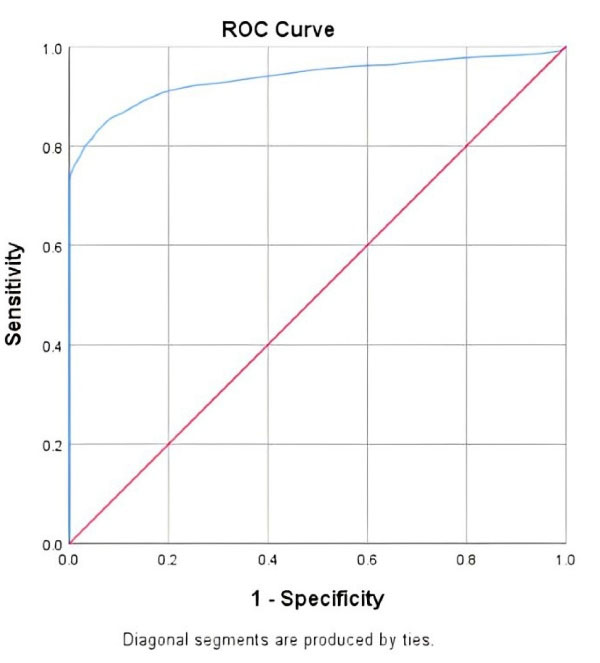
Figure 1.
Rock curve to detect the cutoff point of fasting blood sugar (FBS) in the diagnosis of diabetes
.
Rock curve to detect the cutoff point of fasting blood sugar (FBS) in the diagnosis of diabetes
Discussion
This study aimed to investigate the validity of the self-report of diabetes in a large population in the Yazd region, center of Iran. The results of this study showed that the prevalence of diabetes based on the gold standard was higher than the prevalence of diabetes based on self-report. But this finding shows a slight difference between the prevalence of diabetes based on self-report and the GOLD criteria in this region. So that, the prevalence of diabetes was 18% based on self-report and 19.9% based on the GOLD criteria, which indicated that self-reporting led to an underestimation of diabetes by 9.5%. It could be due to the awareness of the people of this region about diabetes. China Health and Retirement Longitudinal Study (CHARLS) underreporting in self-reported diabetes was 16%.9 Xie and Wang reported that the prevalence of diabetes was 14.25% based on biomedical tests and 8.81% based on self-report.10 Although the difference between self-report and the GOLD criteria in the present study was slight, considering the high prevalence of diabetes in Yazd province, the need for basic measures and more educational programs by health service providers is necessary. In contrast to the results of the present study, a study showed that the prevalence of diabetes based on self-report was higher than the gold standard, which indicated the overestimation of diabetes by the individual.2 Diabetes is a silent disease and its onset is asymptomatic. A person does not know about his illness until he takes the FBS test. Therefore, it seems logical that the prevalence of diabetes based on the gold standard (FBS test...) is higher than self-report. The philosophy of the importance of diabetes screening is also the same as the self-report of diabetes is lower than its actual prevalence in society, so there is a need for diabetes screening in society.
The findings indicated that 1.4% of positive self-reported diabetes was not confirmed by the GOLD criteria. According to the results, about 16% of patients who had diabetes based on the Golden Standard were unaware that they had diabetes, and 22.5% had not received treatment. The results of the STEPs study in 2021 showed that 81.55% of the patients were aware of their disease, which is higher than the national percentage (73.29%).1 Comparison of the results of the STEPS-2021 with the STEPS-2015 shows that the awareness of the people of Yazd province regarding their disease (Diabetes) has increased by 6.76%. In a similar study in the Ravansar cohort, 25.03% of patients who had diabetes based on the Golden Standard were unaware that they had diabetes. It is while 38.78% of the people with a positive self-report; their diabetes was not confirmed according to the GOLD criteria.2
The results of the Moradinazar et al study, which was conducted on a large population, showed that the prevalence of diabetes based on self-report (10.04%) was higher than the GOLD criteria (8.19%).2 In the study conducted in Mashhad, the prevalence of diabetes based on self-report was about 6%, which is lower than the present study.4
The results showed that the accuracy of self-reported diabetes for the correct identification of healthy people from diseased people was 95.67%. As well as the self-reported ability to estimate diseased people (sensitivity = 93.82%) and healthy people (specificity = 96.8%) were high. In the present study, a perfect agreement was between the self-report of diabetes and the GOLD criteria (kappa = 0.86), which indicates the validity of self-reported diabetes to determine the prevalence of diabetes in studies. Meanwhile, the accuracy of self-reported diabetes in the Ravansar cohort study was 0.64, and in the Azar cohort study was 0.66.2,11 The study conducted in Korea also announced the kappa coefficient for diabetes self-report as 0.82%.12
A study conducted in Australia also reported a substantial agreement for self-reported diabetes. Their results indicated the accuracy of self-reported diabetes data in their population.13 Of course, Moradainazar et al believed that agreement depended on socio-demographic variables.2 It is also important to mention that self-reported diabetes is more accurate and valid than other chronic diseases.14 Self-report is more validated in diseases with clear diagnostic criteria (such as the FBS index in diabetes) or diseases with acute outbreaks.15
Of course, a study conducted in China showed that the self-report of diabetes leads to an underestimation of the burden of the disease in society.10 It is also important to mention that the difference in the performance of health systems, economic inequalities, the quality of health education, access to health care,16 and socio-demographic variables of the individual17 are also effective on self-report.
The specificity was higher than the sensitivity in the present study. It is consistent with similar studies.2,4,10,11 In the SHCS, the sensitivity and specificity were higher than in the Ravansar cohort study.2 But the specificity of self-report in the Azar cohort study was more than in the present study.11 The difference in the criteria to determine the GOLD criteria can be the reason for the difference in the results of the studies. For example, in the Azar cohort study, HbA1c was also measured and was part of the GOLD criteria.11 Of course, the quantitative and qualitative increase in people’s awareness of diabetes (due to the high prevalence of diabetes in Yazd province), improving services provided by health care systems, and increase in access to health care are the reasons for higher sensitivity, specificity, and accuracy in the present study compared to similar studies.
In the present study, if the self-report about diabetes was positive, there was an 84% probability that the person had diabetes based on GOLD criteria (PPV). If the self-report was negative, there was a 98% probability that the person was healthy based on GOLD criteria (NPV). The high predictive value indicates the acceptability of people’s self-reports for having or not having a disease and the accuracy of the self-report. The NPV reported in the Ravansar cohort study was 97.7% which is similar to the present study, but the PPV reported in their study was lower than the present study.2 The NPV and PPV were over 90% in the Azar cohort study, were over 95% in a study conducted in Brazil, and were around 90% in Mexico.11,14,18 In the present study, NPV was higher than PPV, which is consistent with other studies conducted.4,11,
In the present study, LR + and LR- were acceptable and suitable. In validation studies, if LR + is greater than 5, the more likely the person with a positive test is truly sick. On the contrary, if the LR- is smaller, the probability of rejecting the presence of the disease using the mentioned test will increase.19
The findings showed that BMI and family history of diabetes in first-degree relatives were related to the disagreement between the GOLD criteria and self-reported diabetes. Thus, a higher BMI and having a family history of diabetes increased the disagreement between the GOLD criteria and self-reported diabetes. These results are consistent with the findings of the Ravansar cohort study.2 In confirmation of these findings, multivariable logistic regression also showed that the odds of over-reporting (false positive) and under-reporting (false negative) in people with normal BMI was lower than in obese people. This finding also applied to family history, so the odds of false positives and negatives were higher in people with a family history of diabetes. It indicates higher odds of disagreement. In Ghorbani et al study, the odds of underreporting diabetes increased with increasing BMI.11 A study conducted in Spain also showed that the odds of false positive self-report was higher in people with a family history of diabetes. The authors believe that this issue is related to the greater awareness of people with a family history of diabetes regarding this disease.20 The results also showed that the odds of under-reporting was higher in smokers, which means that smokers are more likely to think they are healthy while they have diabetes. It may be because smokers are less concerned about their health. One of the limitations of the present study was the lack of measurement of HbA1c in the SHCS. There may also be a recall error.
Conclusion
The findings showed that using self-reported diabetes data to determine the prevalence of diabetes in the study population is valid. Also, there is a perfect agreement between self-reported diabetes and clinical measurements. However, due to the high prevalence of diabetes in society, it seems necessary to increase people’s awareness and conduct primary diabetes screenings.
Competing Interests
The authors declare that there is no conflict of interest.
Ethical Approval
Ethical considerations in this study included obtaining permission from the Ethics Committee of Shahid Sadougi University of Medical Sciences (Ethical Code: IR.SSU.SPH.REC.1399.238).
Research Highlights
What is the current knowledge?
-
The use of the self-report method by researchers to obtain appropriate data is increasing.
-
On the other hand, if the prevalence of the disease is determined based on self-report, the validity of self-report data should be confirmed.
What is new here?
References
- Ministry of Health and Medical Education. Atlas of Non-Communicable Disease Risk Factors Survey in Iran. 2021. Available from: https://nih.tums.ac.ir/UpFiles/Documents/6df47342-c46d-478d-a468-5c1ab0bab710.pdf.
- Moradinazar M, Pasdar Y, Najafi F, Shakiba E, Hamzeh B, Samadi M. Validity of self-reported diabetes varies with sociodemographic charecteristics: example from Iran. Clin Epidemiol Glob Health 2020; 8(1):70-5. doi: 10.1016/j.cegh.2019.04.010 [Crossref] [ Google Scholar]
- Najafi F, Pasdar Y, Shakiba E, Hamzeh B, Darbandi M, Moradinazar M. Validity of self-reported hypertension and factors related to discordance between self-reported and objectively measured hypertension: evidence from a cohort study in Iran. J Prev Med Public Health 2019; 52(2):131-9. doi: 10.3961/jpmph.18.257 [Crossref] [ Google Scholar]
- Barid Kazemi S, Mosa Farkhani E, Eftekhari Gol R, Taghipour A, Bahonar A, Emami O, et al. Validity of self-reported diabetes in a Mashhad population. Iran J Epidemiol.2018; 14(3): 265-71. [Persian].
- Yuan X, Liu T, Wu L, Zou ZY, Li C. Validity of self-reported diabetes among middle-aged and older Chinese adults: the China Health and Retirement Longitudinal Study. BMJ Open 2015; 5(4):e006633. doi: 10.1136/bmjopen-2014-006633 [Crossref] [ Google Scholar]
- Momayyezi M, Fallahzadeh H, Fakhravari L, Mirzaei M. The association between sleep pattern with lipid profile and obesity among adults in Yazd: cross-sectional analysis of Shahedieh Cohort Study. J Nutr Food Secur 2022; 7(3):331-9. doi: 10.18502/jnfs.v7i3.10198 [Crossref] [ Google Scholar]
- Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar AA, Hekmatdoost A. Prospective epidemiological research studies in Iran (the PERSIAN Cohort Study): rationale, objectives, and design. Am J Epidemiol 2018; 187(4):647-55. doi: 10.1093/aje/kwx314 [Crossref] [ Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33(1):159-74. doi: 10.2307/2529310 [Crossref] [ Google Scholar]
- Ning M, Zhang Q, Yang M. Comparison of self-reported and biomedical data on hypertension and diabetes: findings from the China Health and Retirement Longitudinal Study (CHARLS). BMJ Open 2016; 6(1):e009836. doi: 10.1136/bmjopen-2015-009836 [Crossref] [ Google Scholar]
- Xie D, Wang J. Comparison of self-reports and biomedical measurements on hypertension and diabetes among older adults in China. BMC Public Health 2020; 20(1):1664. doi: 10.1186/s12889-020-09770-7 [Crossref] [ Google Scholar]
- Ghorbani Z. Validating Self-Report of Diabetes and Hypertension Use by Participants in the Pilot Phase of Azar Cohort Study: Comparison with Paraclinic Indicators Medical History and Medical Examination [dissertation]. Tabriz University of Medical Sciences, Faculty of Nutrition and Food Sciences; 2018.
- Chun H, Kim IH, Min KD. Accuracy of self-reported hypertension, diabetes, and hypercholesterolemia: analysis of a representative sample of Korean older adults. Osong Public Health Res Perspect 2016; 7(2):108-15. doi: 10.1016/j.phrp.2015.12.002 [Crossref] [ Google Scholar]
- Navin Cristina TJ, Stewart Williams JA, Parkinson L, Sibbritt DW, Byles JE. Identification of diabetes, heart disease, hypertension and stroke in mid- and older-aged women: comparing self-report and administrative hospital data records. Geriatr Gerontol Int 2016; 16(1):95-102. doi: 10.1111/ggi.12442 [Crossref] [ Google Scholar]
- de Mello Fontanelli M, Teixeira JA, Sales CH, de Castro MA, Cesar CL, Alves MC. Validation of self-reported diabetes in a representative sample of São Paulo city. Rev Saude Publica 2017; 51:20. doi: 10.1590/s1518-8787.2017051006378 [Crossref] [ Google Scholar]
- Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 2004; 57(10):1096-103. doi: 10.1016/j.jclinepi.2004.04.005 [Crossref] [ Google Scholar]
- Singh SK, Sharma SK, Mohanty SK, Mishra R, Porwal A, Kishan Gulati B. Inconsistency in prevalence of hypertension based on self-reports and use of standard tests: implications for large scale surveys. SSM Popul Health 2022; 19:101255. doi: 10.1016/j.ssmph.2022.101255 [Crossref] [ Google Scholar]
- Goldman N, Lin IF, Weinstein M, Lin YH. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol 2003; 56(2):148-54. doi: 10.1016/s0895-4356(02)00580-2 [Crossref] [ Google Scholar]
- López-Gómez SA, González-López BS, Scougall-Vilchis RJ, de Lourdes Márquez-Corona M, Minaya-Sánchez M, de Jesús Navarrete-Hernández J. Factors associated with self-report of type 2 diabetes mellitus in adults seeking dental care in a developing country. Int J Environ Res Public Health 2022; 20(1):218. doi: 10.3390/ijerph20010218 [Crossref] [ Google Scholar]
- Grimes DA, Schulz KF. Refining clinical diagnosis with likelihood ratios. Lancet 2005; 365(9469):1500-5. doi: 10.1016/s0140-6736(05)66422-7 [Crossref] [ Google Scholar]
- Soriguer F, Goday A, Bosch-Comas A, Bordiú E, Calle-Pascual A, Carmena R. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the diabetes study. Diabetologia 2012; 55(1):88-93. doi: 10.1007/s00125-011-2336-9 [Crossref] [ Google Scholar]